-
摘要: 目的 :探讨颅底放射性骨髓炎诊治过程,提高诊疗水平。方法 回顾性分析7例鼻咽颅底放射性骨髓炎患者的临床资料,5例为鼻咽癌,1例为蝶窦鳞状细胞癌,1例为腺样囊性癌;6例行鼻咽颅底清创手术,1例放弃手术治疗。结果 术后随访3~31个月(平均11.5个月),2例死亡;1例术后症状部分缓解,随诊时肿瘤复发,同时伴有鼻咽颅底放射性骨髓炎,多学科会诊后建议行靶向减瘤;其余患者手术治疗后症状明显缓解。结论 颅底放射性骨髓炎常合并其他放疗后相关并发症,确诊后应早期行扩大性的颅底清创术,可明显缓解症状,提高生活质量,降低致死性并发症的发生率。
-
关键词:
- 鼻咽颅底放射性骨髓炎 /
- 鼻咽肿瘤 /
- 内镜外科手术
Abstract: Objective To discuss the diagnosis and treatment process of skull base osteoradionecrosis and improve the recognization of this disease.Method We reviewd skull base and nasopharyngeal osteoradionecrosis in 7 patients retrospectively, including 5 nasopharyngeal carcinoma, 1 squamous cell carcinoma of sphenoid sinus, 1 adenoid cystic carcinoma; 6 patientd received skull base debridement surgery and the other one attempted but failed because of her unstable condition.Result Follow-up period ranged from 3 to 31 months (mean 11.5 month). During the review time, 2 patients died, 1 patient still had osteoradionecrosis with partly alleviated clinical symptom. At the latest follow-up visit, she was diagnosed as tumor recurrence and was advised to take targeted therapy by multi-discipline team; the symptom was significant improved in the rest of the patients.Conclusion Osteoradionecrosis of skull base is often associated with other post-radiotherapy related complications. Once diagnosed definitely, extensive skull base debridement surgery should be performed in early time, which can significantly relieve symptoms, improve living quality and reduce the incidence of lethal complications. -

-
表 1 7例患者的一般资料
例序 性别 年龄/岁 既往史(包括手术史、放化疗史) 病理类型 放疗后并发症或合并症 随访结果 1 男 58 ①诱导化疗3个周期:每个周期多西他赛120 mg,顺铂120 mg;②同期放化疗:靶区总剂量73.26 Gy;同期化疗2个周期,每个周期顺铂160 mg 鼻咽部非角化性癌未分化型 肺部感染:铜绿假单胞菌 因咽旁间隙感染死亡 2 女 58 根治性放化疗:①调强放疗:靶区总剂量74.25 Gy;②化疗增敏3个周期:每个周期顺铂150mg 鼻咽非角化性癌分化型 头皮脓肿、多脏器功能衰竭 因多脏器功能衰竭死亡 3 女 40 2011年确诊并放疗(放疗史不详);2015年因复发再次行放化疗及手术治疗(具体不详);2018年行鼻内镜下鼻咽颅底斜坡双咽旁翼腭窝肿物扩大切除,左股内侧皮肤切取移植 鼻咽癌非角化性癌未分化型 张口受限 头痛部分缓解 4 男 61 放疗38次(剂量不详),化疗2次(奈达铂,剂量不详) 蝶窦鳞状细胞癌 继发腺垂体功能减退 治愈 5 女 66 2013年行右侧蝶窦底壁、嗅裂、鼻咽部、鼻中隔肿物扩大切除,术后放疗(剂量不详) 鼻腔鼻窦腺样囊性癌 无 头痛部分缓解 6 男 49 化疗3个周期:每个周期顺铂120 mg,氟脲苷3 750 mg,亚叶酸钙1 000 mg;右侧Ⅱ、Ⅲ、Ⅴ区颈部淋巴结清扫;调强放疗:靶区总剂量70 Gy,生物制剂免疫治疗;同步放化疗:靶区总剂量70.4 Gy,同步化疗顺铂60 mg,甘胺双咗钠放疗增敏 鼻咽低分化鳞状细胞癌 亚临床甲状腺功能减退,咽旁间隙炎 头痛部分缓解,需用布洛芬缓解,2片/d,用量减少(术前3~4片/d) 7 女 63 同期放化疗:放疗靶区总剂量73.26 Gy;化疗1个周期,顺铂100 mg 鼻咽癌非角化性癌未分化型 无 头痛治愈;继发肺转移 表 2 颅底放射性骨髓炎及颅骨骨髓炎比较
鼻咽颅底放射性骨髓炎 颅骨骨髓炎 病因 放疗、损伤、感染 ①感染因素:多见于坏死性外耳道炎、慢性乳突炎、蝶窦炎;②手术因素;③创伤;④系统性疾病 致病机制 放疗因素导致组织内血管减少,氧供不足,组织细胞减少 细菌杀伤与抗菌平衡打破 易感因素 头颈部肿瘤患者接受放疗后 局部慢性炎症继发感染,全身情况差,见于糖尿病、免疫缺陷等患者 感染关系 局部黏膜组织坏死后继发感染 感染在致病过程中起主导因素 临床表现 鼻部恶臭、头痛、鼻出血 耳痛、发热、耳闷胀感、耳流脓、头痛、颞颌关节痛 治疗方法 鼻腔冲洗,根据细菌培养及药敏结果口服或静脉滴注抗生素,应用黏膜促排剂,高压氧治疗 大剂量长疗程抗生素静脉滴注,手术治疗,高压氧治疗 -
[1] Khan MA, Quadri SAQ, Kazmi AS, et al. A Comprehensive Review of Skull Base Osteomyelitis: Diagnostic and Therapeutic Challenges among Various Presentations[J]. Asian J Neurosurg, 2018, 13(4): 959-970. doi: 10.4103/ajns.AJNS_90_17
[2] Marx RE. Osteoradionecrosis: a new concept of its pathophysiology[J]. J Oral Maxillofac Surg, 1983, 41(5): 283-288. doi: 10.1016/0278-2391(83)90294-X
[3] Lee CC, Ho CY. Post-treatment late complications of nasopharyngeal carcinoma[J]. Eur Arch Otorhinolaryngol, 2012, 269(11): 2401-2409. doi: 10.1007/s00405-011-1922-2
[4] Han P, Wang X, Liang F, et al. Osteoradionecrosis of the Skull Base in Nasopharyngeal Carcinoma: Incidence and Risk Factors[J]. Int J Radiat Oncol Biol Phys, 2018, 102(3): 552-555. doi: 10.1016/j.ijrobp.2018.06.027
[5] Lee IJ, Koom WS, Lee CG, et al. Risk factors and dose-effect relationship for mandibular osteoradionecrosis in oral and oropharyngeal cancer patients[J]. Int J Radiat Oncol Biol Phys, 2009, 75(4): 1084-1091. doi: 10.1016/j.ijrobp.2008.12.052
[6] Silvestre-Rangil J, Silvestre FJ. Clinico-therapeutic management of osteoradionecrosis: a literature review and update[J]. Med Oral Patol Oral Cir Bucal, 2011, 16(7): e900-e904.
[7] Bedwinek JM, Shukovsky LJ, Fletcher GH, et al. Osteonecrosis in patients treated with definitive radiotherapy for squamous cell carcinomas of the oral cavity and naso-and oropharynx[J]. Radiology, 1976, 119(3): 665-667. doi: 10.1148/119.3.665
[8] King AD, Griffith JF, Abrigo JM, et al. Osteoradionecrosis of the upper cervical spine: MR imaging following radiotherapy for nasopharyngeal carcinoma[J]. Eur J Radiol, 2010, 73(3): 629-635. doi: 10.1016/j.ejrad.2008.12.016
[9] Lalani N, Huang SH, Rotstein C, et al. Skull base or cervical vertebral osteomyelitis following chemoradiotherapy for pharyngeal carcinoma: A serious but treatable complication[J]. Clin Transl Radiat Oncol, 2017, 8: 40-44.
[10] Huang XM, Zheng YQ, Zhang XM, et al. Diagnosis and management of skull base osteoradionecrosis after radiotherapy for nasopharyngeal carcinoma[J]. Laryngoscope, 2006, 116(9): 1626-1631. doi: 10.1097/01.mlg.0000230435.71328.b9
[11] Cheung JP, Wei WI, Luk KD. Cervical spine complications after treatment of nasopharyngeal carcinoma[J]. Eur Spine J, 2013, 22(3): 584-592. doi: 10.1007/s00586-012-2600-9
[12] Siegmund BJ, Rustemeyer J. Case report: chronic inflammatory ulcer and osteoradionecrosis of the skull following radiotherapy in early childhood[J]. Oral Maxillofac Surg, 2019, 23(2): 239-246. doi: 10.1007/s10006-019-00752-7
[13] Ogura I, Sasaki Y, Sue M, et al. Tc-99 m hydroxymethylene diphosphonate scintigraphy, computed tomography, and magnetic resonance imaging of osteonecrosis in the mandible: Osteoradionecrosis versus medication-related osteonecrosis of the jaw[J]. Imaging Sci Dent, 2019, 49(1): 53-58. doi: 10.5624/isd.2019.49.1.53
[14] Hao SP, Tsang NM, Chang KP. Differentiation of recurrent nasopharyngeal carcinoma and skull base osteoradionecrosis by Epstein-Barr virus-derived latent membrane protein-1 gene[J]. Laryngoscope, 2001, 111(4 Pt 1): 650-652.
[15] Labib MA, Prevedello DM, Carrau R, et al. A road map to the internal carotid artery in expanded endoscopic endonasal approaches to the ventral cranial base[J]. Neurosurgery, 2014, 10 Suppl 3: 448-471.
[16] Abdulrauf SI, Ashour AM, Marvin E, et al. Proposed clinical internal carotid artery classification system[J]. J Craniovertebr Junction Spine, 2016, 7(3): 161-170. doi: 10.4103/0974-8237.188412
[17] Adel M, Chang KP. Using a nasoseptal flap for the reconstruction of osteoradionecrosis in nasopharyngeal carcinoma: a case report[J]. J Otolaryngol Head Neck Surg, 2016, 45: 27. doi: 10.1186/s40463-016-0139-1
[18] Fortes FS, Carrau RL, Snyderman CH, et al. Transpterygoid transposition of a temporoparietal fascia flap: a new method for skull base reconstruction after endoscopic expanded endonasal approaches[J]. Laryngoscope, 2007, 117(6): 970-976. doi: 10.1097/MLG.0b013e3180471482
[19] Liu J, Ning X, Sun X, et al. Endoscopic sequestrectomy for skull base osteoradionecrosis in nasopharyngeal carcinoma patients: a 10year experience[J]. Int J Clin Oncol, 2019, 24(3): 248-255. doi: 10.1007/s10147-018-1354-8
-

| 引用本文: | 赵天峰, 石照辉, 许敏, 等. 鼻咽颅底放射性骨髓炎临床分析[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(5): 436-440. doi: 10.13201/j.issn.2096-7993.2020.05.012 |
| Citation: | ZHAO Tianfeng, SHI Zhaohui, XU Min, et al. Osteoradionecrosis of skull base: clinical analysis and experience[J]. J Clin Otorhinolaryngol Head Neck Surg, 2020, 34(5): 436-440. doi: 10.13201/j.issn.2096-7993.2020.05.012 |
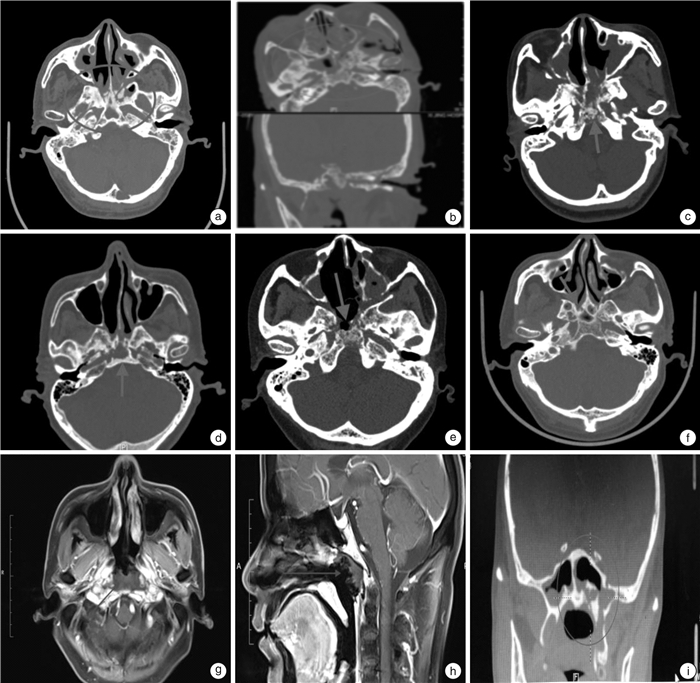
- Figure 1.



 下载:
下载: