Comparative analysis of surgical methods for parathyroidectomy and forearm transplantation in secondary hyperparathyroidism
-
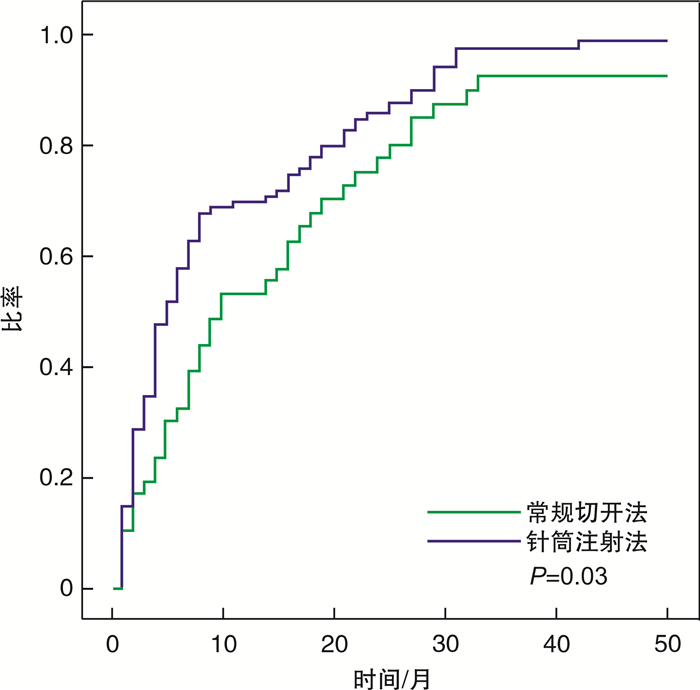
摘要: 目的 比较继发性甲状旁腺功能亢进患者接受甲状旁腺全切除后,采用改良的针筒前臂定量注射法与前臂切口肱桡肌内移植法的疗效。方法 接受甲状旁腺全切除的继发性甲状旁腺功能亢进患者152例,按照术中不同的前臂移植甲状旁腺方式分为肱桡肌切开移植组和针筒前臂定量移植组。统计手术操作时长、术前术后甲状旁腺激素水平、血钙等指标并进行对照分析。结果 2组患者在实验室检查方面差异无统计学意义,但改良的针筒前臂定量注射法操作更为便捷,针筒前臂定量移植组术后甲状旁腺激素水平恢复时间(3个月)较肱桡肌切开移植组(6个月)更短(P=0.03)。2组患者在移植后复发情况的差异无统计学意义。结论 改良的针筒前臂定量注射法移植甲状旁腺,操作相对简单、更节省时间、可使移植的甲状旁腺更快发挥功能,值得广泛运用。
-
关键词:
- 继发性甲状旁腺功能亢进 /
- 甲状旁腺切除术 /
- 自体移植
Abstract: Objective To compare the different therapeutic effects of modified syringe forearm quantitative injection and forearm brachioradialis intramuscular transplantation after receiving total parathyroidectomy in patients with secondary hyperparathyroidism.Method One hundred and fifty-two patients with secondary hyperparathyroidism who underwent total parathyroidectomy were divided into the forearm brachioradialis intramuscular transplantation group and the modified syringe forearm quantitative injection group according to the different forearm transplantation methods. The study counted and compared the duration of surgery, preoperative and postoperative parathyroid hormone levels, blood calcium and other indicators.Result The results showed that there was no statistically significant difference in laboratory test data between the two groups, but the modified syringe forearm quantitative injection method was more convenient, and the recovery time of the parathyroid function was shortened from an average of 6 months to an average of 3 months(P=0.03). There was no statistical difference in the recurrence of the two groups of patients after transplantation.Conclusion The modified syringe forearm quantitative injection method for transplantation of parathyroid gland is relatively simple to operate, saves time, and enables the transplanted parathyroid gland to function faster. It is worthy of being widely used.-
Key words:
- secondary hyperparathyroidism /
- parathyroidectomy /
- autotransplantation
-

-
表 1 针筒前臂定量移植组和肱桡肌切开移植组临床及实验室数据比较
临床及检查项目 针筒前臂定量移植 肱桡肌切开移植 P值 例数 100 42 年龄/岁 55(35~74) 56(39~75) 0.297 性别 0.352 男 46(46.0) 17(40.5) 女 54(54.0) 25(59.5) 透析方式 0.471 血透 82(82.0) 35(83.3) 腹透 17(17.0) 7(16.7) 不明 1(1.0) 0(0) 透析年限/年 8(1~23) 7(2~30) 0.442 手术用时/min 99(60~252) 107(60~240) 0.352 术前PTH/(pg·ml-1) 1 324(347~2 500) 1 204(390~2 500) 0.243 术后PTH/(pg·ml-1) 0.287 < 12 62(62.0) 24(57.1) 12~72 29(29.0) 13(31.0) >72~300 6(6.0) 2(4.8) >300 3(3.0) 3(7.1) 术前校正血钙/(mmol·L-1) 2.74(2.23~3.75) 2.76(2.45~3.33) 0.591 术后校正血钙/(mmol·L-1) 2.47(2.08~3.44) 2.45(1.95~2.94) 0.214 术后葡萄糖酸钙静脉用量/g 8(6~26) 9(6~27) 0.397 -
[1] 张凌. 继发性甲状旁腺功能亢进的治疗策略[J]. 中华肾病研究电子杂志, 2015, 4(3): 5-9. https://www.cnki.com.cn/Article/CJFDTOTAL-SHSB201503003.htm
[2] Bilezikian JP, Bandeira L, Khan A, et al. Hyperparathyroidism[J]. Lancet, 2018, 391(10116): 168-178. doi: 10.1016/S0140-6736(17)31430-7
[3] Uhlig K, Berns JS, Kestenbaum B, et al. KDOQI US commentary on the 2009 KDIGO clinical practice guideline for the diagnosis, evaluation, and treatment of CKD-mineral and bone disorder(CKD-MBD)[J]. Am J Kidney Dis, 2010, 55(5): 773-799. doi: 10.1053/j.ajkd.2010.02.340
[4] Ng JC, Wang W, Chua MJ, et al. Subcutaneous injection is a simple and reproducible option to restore parathyroid function after total parathyroidectomy in patients with secondary hyperparathyroidism[J]. Surgery, 2014, 155(4): 682-688. doi: 10.1016/j.surg.2013.12.019
[5] Anderson K Jr, Ruel E, Adam MA, et al. Subtotal vs. total parathyroidectomy with autotransplantation for patients with renal hyperparathyroidism have similar outcomes[J]. Am J Surg, 2017, 214(5): 914-919. doi: 10.1016/j.amjsurg.2017.07.018
[6] Lorenz K, Bartsch DK, Sancho JJ, et al. Surgical management of secondary hyperparathyroidism in chronic kidney disease—a consensus report of the European Society of Endocrine Surgeons[J]. Langenbecks Arch Surg, 2015, 400(8): 907-927. doi: 10.1007/s00423-015-1344-5
[7] Madorin C, Owen RP, Fraser WD, et al. The surgical management of renal hyperparathyroidism[J]. Eur Arch Otorhinolaryngol, 2012, 269(6): 1565-1576. doi: 10.1007/s00405-011-1833-2
[8] Schlosser K, Bartsch DK, Diener MK, et al. Total parathyroidectomy with routine thymectomy and autotransplantation versus total parathyroidectomy alone for secondary hyperparathyroidism[J]. Ann Surg, 2016, 264(5): 745-753. doi: 10.1097/SLA.0000000000001875
[9] 殷德涛, 余坤. 继发性甲状旁腺功能亢进症的外科治疗[J]. 中国普通外科杂志, 2016, 25(5): 631-634. https://www.cnki.com.cn/Article/CJFDTOTAL-ZPWZ201605001.htm
[10] Hsu YC, Hung CJ. Intramuscular and subcutaneous forearm parathyroid autograft hyperplasia in renal dialysis patients: A retrospective cohort study[J]. Surgery, 2015, 158(5): 1331-1338. doi: 10.1016/j.surg.2015.04.027
[11] Gopalakrishna NI, Shaha AR. Complications of thyroid surgery: prevention and management[J]. Minerva Chir, 2010, 65(1): 71-82.
[12] Tominaga Y, Matsuoka S, Uno N, et al. Removal of autografted parathyroid tissue for recurrent renal hyperparathyroidism in hemodialysis patients[J]. World J Surg, 2010, 34(6): 1312-1317. doi: 10.1007/s00268-010-0412-9
[13] Agha A, Loss M, Schlitt HJ, et al. Recurrence of secondary hyperparathyroidism in patients after total parathyroidectomy with autotransplantation: technical and therapeutic aspects[J]. Eur Arch Otorhinolaryngol, 2012, 269(5): 1519-1525. doi: 10.1007/s00405-011-1776-7
[14] Messa P, Castelnovo C, Scalamogna A. Calcimimetics in peritoneal dialysis patients[J]. Contrib Nephrol, 2012, 178: 143-149. doi: 10.1159/000337834
-





 下载:
下载: