Prognostic value of olfactory bulb volume in patients with post-viral olfactory dysfunction
-
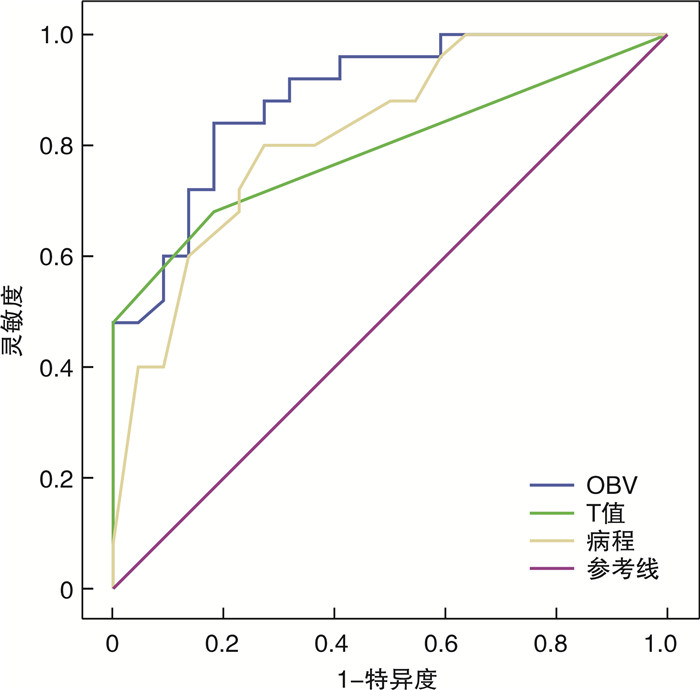
摘要: 目的 比较上呼吸道感染后嗅觉障碍(PVOD)患者不同预后组间的嗅觉功能检查结果,分析预后相关因素,尤其嗅球体积(OBV)对预后的影响,为临床诊疗提供客观依据。方法 对2019年1月—2019年12月于北京安贞医院门诊就诊的PVOD患者进行≥1年的随访,这些患者在治疗前完成Sniffin'Sticks嗅觉测试、嗅通路MRI检查。根据1年随访期后Sniffin'Sticks嗅觉测试结果总分提高≥6分,将患者分为嗅觉功能改善组和嗅觉功能无改善组。比较两组间各因素和嗅觉功能检查结果的差异,初步确定影响PVOD患者的预后因素。结果 共纳入47例PVOD患者,Sniffin'Sticks嗅觉测试复查结果显示嗅觉改善率为53.2%。与嗅觉功能改善组相比,嗅觉功能无改善组患者病程长,初始嗅觉功能差,嗅觉阈值高,嗅觉辨别和识别能力差(均P < 0.01)。两组在性别、年龄、变应性鼻炎和吸烟方面差异均无统计学意义(均P>0.05)。嗅觉功能无改善组的OBV为(59.48±23.92) mm3,明显小于嗅觉功能改善组[(92.77±14.35) mm3]。经多元logistic回归分析预后相关因素包括病程(OR 0.677,95%CI 0.461~0.993,P=0.046),初始T值(OR 263.806,95%CI 1.028~67 675.884,P=0.049)和OBV(OR 1.160,95%CI 1.002~1.343,P=0.047)。ROC曲线分析结果显示,OBV在ROC曲线下面积为0.888(0.797~0.979,P < 0.001),以OBV≥78.50 mm3正确诊断指数判断嗅觉功能预后良好,其特异性为0.818,敏感性为0.840;病程因素ROC曲线下面积为0.822(0.703~0.940,P < 0.001),以病程≤6个月为正确诊断指数判断嗅觉功能预后良好,其特异性为0.727,敏感性为0.800;T值ROC曲线下面积为0.793(0.662~0.924,P=0.001),以T值≥1.25为正确诊断指数判断嗅觉功能预后较好,其特异性为0.818,敏感性为0.680。结论 PVOD患者嗅觉功能预后与病程、嗅觉损伤程度和OBV有关。嗅觉功能无改善者较嗅觉功能改善者病程延长,嗅觉损伤程度加重和OBV减小。病程≤6个月,T值≥1.25和OBV≥78.50 mm3均提示预后良好,且客观嗅觉检查结果对嗅觉功能预后的评估价值更大。
-
关键词:
- 上呼吸道感染后嗅觉障碍 /
- 嗅球体积 /
- 预后 /
- Sniffin'Sticks测试 /
- 嗅觉训练
Abstract: Objective The purpose of this study was to compare the olfactory function examination results of patients with post-viral olfactory dysfunction(PVOD) in different prognostic groups and analyze prognostic factors, especially the influence of olfactory bulb volume(OBV) on prognosis, so as to provide objective basis for clinical diagnosis and treatment.Methods After approval by the hospital ethics committee, the patients with PVOD admitted to Beijing Anzhen Hospital's outpatient department from January 2019 to December 2019 were followed up for at least 1 year. These patients completed the Sniffin' Sticks test and MRI examination of the olfactory pathway before treatment. According to the results of the Sniffin' Sticks test after 1 year follow-up(threshold-discrimination-identification(TDI) score of the patients was increased at least 6 points), the patients were divided into two groups as the improvement group and the non-improvement group. The prognostic factors of PVOD patients were preliminarily determined by comparing the differences of various factors and the results of olfactory function examination between the two groups.Results In this study, 47 patients with PVOD were included, with the smell improvement rate was 53.2%. Compared with the improvement group, the patients in the non-improvement group had longer duration, poorer initial olfactory function, higher olfactory threshold, and poorer olfactory discrimination and recognition ability(All P < 0.01). There was no statistical difference in terms of gender, age, allergic rhinitis and smoking between the two groups(All P>0.05).The OBV of the non-improvement group was (59.48±23.92) mm3, which was significantly lower than that in the improvement group([92.77±14.35]mm3, P < 0.001). Multiple logistic regression analysis showed that prognostic factors included course of disease(OR 0.677, 95%CI 0.461-0.993, P=0.046), initial T value(OR 263.806, 95%CI 1.028-67 675.884, P=0.049) and OBV(OR 1.160, 95%CI 1.002-1.343, P=0.047). The area under the receiver operating characteristic curve(ROC curve) of OBV was 0.888(0.797-0.979, P < 0.001). The correct diagnostic index of OBV≥78.50 mm3was used to determine the prognosis of olfactory function, with a specificity of 0.818 and a sensitivity of 0.840. The ROC curve analysis showed that the area under the ROC curve of duration was 0.822(0.703-0.940, P < 0.001). The correct diagnostic index of the duration ≤6 months was used to determine the prognosis of olfactory function, with a specificity of 0.727 and a sensitivity of 0.800. The area of T score was 0.793(0.662-0.924, P=0.001). T score ≥1.25 was used as the correct diagnostic index to determine the prognosis of olfactory function. The specificity and sensitivity were 0.818 and 0.680, respectively.Conclusion The prognosis of olfactory function in PVOD patients is related to the course of disease, the degree of olfactory loss and OBV. Those with no improvement in olfactory function have a longer disease course, aggravated olfactory damage and reduced OBV than those with improved olfactory function. The factors of Duration ≤6 months, T value ≥1.25 and OBV≥78.50 mm3suggested better prognosis, and the results of objective olfactory examination have greater value in evaluating the prognosis of olfactory function. -

-
表 1 嗅觉训练使用气味
名称 CAS号 类别 苯乙醇 60-12-8 ≥99% 薄荷醇 2216-51-5 ≥99% 香茅醛 106-23-0 ≥99% 丁香酚 97-53-0 ≥99% 表 2 嗅觉功能改善组和嗅觉功能无改善组患者各因素比较
因素 嗅觉功能改善组(n=25) 嗅觉功能无改善组(n=22) P值 年龄/岁a) 45.00±12.09 45.55±15.40 0.541 男性/例(%) 7(28.00) 7(31.82) 0.512 病程/月b) 2.5(1~12) 8.75(1.5~72) < 0.001 变应性鼻炎/例(%) 14(56.00) 10(45.45) 0.334 吸烟/例(%) 7(28.00) 8(36.36) 0.381 治疗前TDIa) 16.84±4.86 9.86±5.12 < 0.001 治疗前T值b) 1.5(1~4.5) 1(1~1.5) < 0.001 治疗前D值a) 7.24±2.47 4.95±3.06 0.007 治疗前I值a) 7.80±2.97 4.32±2.44 < 0.001 随访TDIa) 25.58±5.76 12.81±4.55 < 0.001 随访T值a) 4.06±1.82 1.85±0.93 < 0.001 随访D值a) 10.16±2.34 5.59±1.44 < 0.001 随访I值a) 11.40±2.16 5.73±2.37 < 0.001 OBV/mm3 92.77±14.35 59.48±23.92 < 0.001 注:a)x±S;b)中位数(范围)。 表 3 PVOD患者不同嗅觉功能损伤程度恢复情况
时间 损伤程度 PVOD 嗅觉功能改善组(n=25) 嗅觉功能无改善组(n=22) 治疗前 失嗅 29 9 20 嗅觉减退 18 16 2 治疗后 失嗅 18 2 16 嗅觉减退 24 18 6 嗅觉功能正常 5 5 0 表 4 PVOD患者各因素多元logistics回归分析
因素 OR 95%CI β P值 病程 0.677 0.461~0.993 -0.391 0.046 治疗前T值 263.806 1.028~67 675.884 5.575 0.049 治疗前D值 27.373 0.891~840.962 3.310 0.058 治疗前I值 33.555 0.914~1232.052 3.513 0.056 治疗前TDI 0.036 0.001~1.188 -3.330 0.062 OBV 1.160 1.002~1.343 0.148 0.047 -
[1] Pinto JM, Wroblewski KE, Kern DW, et al. Olfactory dysfunction predicts 5-year mortality in older adults[J]. PLoS One, 2014, 9(10): e107541. doi: 10.1371/journal.pone.0107541
[2] Van Regemorter V, Hummel T, Rosenzweig F, et al. Mechanisms Linking Olfactory Impairment and Risk of Mortality[J]. Front Neurosci, 2020, 14: 140. doi: 10.3389/fnins.2020.00140
[3] Rawal S, Hoffman HJ, Bainbridge KE, et al. Prevalence and Risk Factors of Self-Reported Smell and Taste Alterations: Results from the 2011-2012 US National Health and Nutrition Examination Survey(NHANES)[J]. Chem Senses, 2016, 41(1): 69-76. doi: 10.1093/chemse/bjv057
[4] Nordin S, Brämerson A. Complaints of olfactory disorders: epidemiology, assessment and clinical implications[J]. Curr Opin Allergy Clin Immunol, 2008, 8(1): 10-15. doi: 10.1097/ACI.0b013e3282f3f473
[5] Chen G, Wei Y, Miao X, et al. Clinical features of olfactory disorders in patients seeking medical consultation[J]. Med Sci Monit, 2013, 19: 444-450. doi: 10.12659/MSM.883938
[6] 魏永祥, 刘钢, 刘剑锋, 等. 嗅觉障碍诊断和治疗专家共识(2017年)[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(7): 484-494. doi: 10.3760/cma.j.issn.1673-0860.2018.07.002
[7] Jung YG, Lee JS, Park GC. Does post-infectious olfactory loss affect mood more severely than chronic sinusitis with olfactory loss?[J]. Laryngoscope, 2014, 124(11): 2456-2460. doi: 10.1002/lary.24691
[8] Hura N, Xie DX, Choby GW, et al. Treatment of post-viral olfactory dysfunction: an evidence-based review with recommendations[J]. Int Forum Allergy Rhinol, 2020, 10(9): 1065-1086. doi: 10.1002/alr.22624
[9] Kattar N, Do TM, Unis GD, et al. Olfactory Training for Postviral Olfactory Dysfunction: Systematic Review and Meta-analysis[J]. Otolaryngol Head Neck Surg, 2021, 164(2): 244-254. doi: 10.1177/0194599820943550
[10] Potter MR, Chen JH, Lobban NS, et al. Olfactory dysfunction from acute upper respiratory infections: relationship to season of onset[J]. Int Forum Allergy Rhinol, 2020, 10(6): 706-712. doi: 10.1002/alr.22551
[11] Tian J, Pinto JM, Li L, et al. Identification of Viruses in Patients With Postviral Olfactory Dysfunction by Multiplex Reverse-Transcription Polymerase Chain Reaction[J]. Laryngoscope, 2021, 131(1): 158-164. doi: 10.1002/lary.28997
[12] 田俊, 魏永祥. 上气道感染后嗅觉障碍病因及其致病机制研究进展[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(5): 477-480. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201905026.htm
[13] Fornazieri MA, Garcia E, Lopes N, et al. Adherence and Efficacy of Olfactory Training as a Treatment for Persistent Olfactory Loss[J]. Am J Rhinol Allergy, 2020, 34(2): 238-248. doi: 10.1177/1945892419887895
[14] Rombaux P, Huart C, Deggouj N, et al. Prognostic value of olfactory bulb volume measurement for recovery in postinfectious and posttraumatic olfactory loss[J]. Otolaryngol Head Neck Surg, 2012, 147(6): 1136-1141. doi: 10.1177/0194599812459704
[15] Hummel T, Sekinger B, Wolf SR, et al. 'Sniffin' sticks': olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold[J]. Chem Senses, 1997, 22(1): 39-52. doi: 10.1093/chemse/22.1.39
[16] Hummel T, Lötsch J. Prognostic factors of olfactory dysfunction[J]. Arch Otolaryngol Head Neck Surg, 2010, 136(4): 347-351. doi: 10.1001/archoto.2010.27
[17] Hummel T, Rissom K, Reden J, et al. Effects of olfactory training in patients with olfactory loss[J]. Laryngoscope, 2009, 119(3): 496-499. doi: 10.1002/lary.20101
[18] 闫晓光, 高星, 孙智甫, 等. 嗅觉训练治疗嗅觉障碍的临床疗效和影响因素分析[J]. 中华耳鼻咽喉头颈外科杂志, 2018, 53(11): 815-819. doi: 10.3760/cma.j.issn.1673-0860.2018.11.004
[19] Kim DH, Kim SW, Hwang SH, et al. Prognosis of Olfactory Dysfunction according to Etiology and Timing of Treatment[J]. Otolaryngol Head Neck Surg, 2017, 156(2): 371-377. doi: 10.1177/0194599816679952
[20] Altundag A, Cayonu M, Kayabasoglu G, et al. Modified olfactory training in patients with postinfectious olfactory loss[J]. Laryngoscope, 2015, 125(8): 1763-1766. doi: 10.1002/lary.25245
[21] London B, Nabet B, Fisher AR, et al. Predictors of prognosis in patients with olfactory disturbance[J]. Ann Neurol, 2008, 63(2): 159-166. doi: 10.1002/ana.21293
[22] Lee DY, Lee WH, Wee JH, et al. Prognosis of postviral olfactory loss: follow-up study for longer than one year[J]. Am J Rhinol Allergy, 2014, 28(5): 419-422. doi: 10.2500/ajra.2014.28.4102
[23] Reden J, Mueller A, Mueller C, et al. Recovery of olfactory function following closed head injury or infections of the upper respiratory tract[J]. Arch Otolaryngol Head Neck Surg, 2006, 132(3): 265-269. doi: 10.1001/archotol.132.3.265
[24] Hedner M, Larsson M, Arnold N, et al. Cognitive factors in odor detection, odor discrimination, and odor identification tasks[J]. J Clin Exp Neuropsychol, 2010, 32(10): 1062-1067. doi: 10.1080/13803391003683070
[25] Haehner A, Rodewald A, Gerber JC, et al. Correlation of olfactory function with changes in the volume of the human olfactory bulb[J]. Arch Otolaryngol Head Neck Surg, 2008, 134(6): 621-624. doi: 10.1001/archotol.134.6.621
[26] 苏百晗, 孙智甫, 陈忠维, 等. 18F-FDG用于评估外伤性嗅神经损伤对药物经鼻脑通路运输的影响[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(12): 1148-1152. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201912009.htm
[27] Gottfried JA. Central mechanisms of odour object perception[J]. Nat Rev Neurosci, 2010, 11(9): 628-641. doi: 10.1038/nrn2883
[28] Gottfried JA, Zald DH. On the scent of human olfactory orbitofrontal cortex: meta-analysis and comparison to non-human primates[J]. Brain Res Brain Res Rev, 2005, 50(2): 287-304. doi: 10.1016/j.brainresrev.2005.08.004
[29] Fjaeldstad A, Fernandes HM, Van Hartevelt TJ, et al. Brain fingerprints of olfaction: a novel structural method for assessing olfactory cortical networks in health and disease[J]. Sci Rep, 2017, 7: 42534. doi: 10.1038/srep42534
[30] Zhou G, Lane G, Cooper SL, et al. Characterizing functional pathways of the human olfactory system[J]. Elife, 2019, 8: e47177. doi: 10.7554/eLife.47177
[31] Bauknecht HC, Jach C, Fleiner F, et al. [Olfactory dysfunction: correlation of olfactory bulb volume on MRI and objective olfactometry][J]. Rofo, 2010, 182(2): 163-168. doi: 10.1055/s-0028-1109816
[32] Mueller A, Rodewald A, Reden J, et al. Reduced olfactory bulb volume in post-traumatic and post-infectious olfactory dysfunction[J]. Neuroreport, 2005, 16(5): 475-478. doi: 10.1097/00001756-200504040-00011
[33] Manan HA, Yahya N, Han P, et al. A systematic review of olfactory-related brain structural changes in patients with congenital or acquired anosmia[J]. Brain Struct Funct, 2021, 12: 1-26. https://pubmed.ncbi.nlm.nih.gov/34635958/
[34] Rombaux P, Mouraux A, Bertrand B, et al. Olfactory function and olfactory bulb volume in patients with postinfectious olfactory loss[J]. Laryngoscope, 2006, 116(3): 436-439. doi: 10.1097/01.MLG.0000195291.36641.1E
[35] Yao L, Yi X, Pinto JM, et al. Olfactory cortex and Olfactory bulb volume alterations in patients with post-infectious Olfactory loss[J]. Brain Imaging Behav, 2018, 12(5): 1355-1362. doi: 10.1007/s11682-017-9807-7
[36] Hummel T, Urbig A, Huart C, et al. Volume of olfactory bulb and depth of olfactory sulcus in 378 consecutive patients with olfactory loss[J]. J Neurol, 2015, 262(4): 1046-1051. doi: 10.1007/s00415-015-7691-x
-




 下载:
下载: