Radiofrequency ablation of inferior turbinate in the treatment of allergic rhinitis in children
-
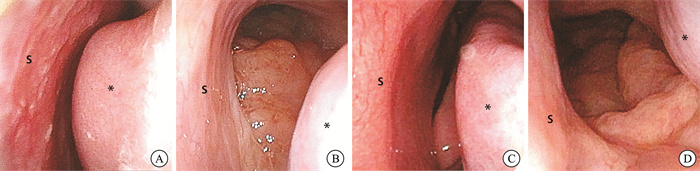
摘要: 目的 探讨下鼻甲黏膜下射频消融术的安全性和有效性,为儿童变应性鼻炎(AR)的外科治疗提供临床依据。方法 研究纳入2021年1月—2023年12月收治于上海市儿童医院耳鼻咽喉头颈外科并接受双侧下鼻甲黏膜下射频消融术,同时接受腺样体扁桃体射频消融的伴有AR的阻塞性睡眠呼吸暂停低通气综合征的患儿。通过观察指标和统计学方法对疗效进行评估。结果 本研究共纳入病例51例,其中43例进行了半年的随访。下鼻甲黏膜下射频消融术+腺样体扁桃体射频消融术取得了良好的疗效,总有效率为93%。患儿术前术后的症状差异有统计学意义(P<0.05)。无出血、咽鼓管损伤、鼻腔粘连、鼻腔干燥等并发症发生。结论 在严格控制手术适应证的前提下,儿童AR可以采用外科手术进行治疗。其中,下鼻甲黏膜下射频消融术更微创,且具有良好的有效性和安全性,可在临床推广应用。Abstract: Objective To investigate the safety and efficacy of submucous radiofrequency ablation of the inferior turbinate, and to provide a clinical basis for the surgical treatment of allergic rhinitis in children.Methods Patients with obstructive sleep apnea syndrome and allergic rhinitis who were admitted to the Department of Otolaryngology Head and Neck Surgery of Shanghai Children's Hospital from January 2021 to December 2023 and underwent bilateral submucous radiofrequency ablation of the inferior turbinate and radiofrequency ablation of the adenoid tonsil were included in the study. Observational and statistical indexes were used to evaluate the curative effect.Results A total of 51 cases were included in this study, and 43 cases were followed up for half a year. Submucous radiofrequency ablation of the inferior turbinate plus radiofrequency ablation of the adenoid tonsil achieved a good effect (total effective rate 93%), and there was a statistically significant difference in the preoperative and postoperative symptoms of the children(P<0.05). There were no complications such as bleeding, Eustachian tube injury, nasal adhesion, or nasal dryness.Conclusion Under the premise of strict control of surgical indications, children with allergic rhinitis can be treated surgically. Inferior turbinate submucous radiofrequency ablation is more minimally invasive, effective, and safe, and can be used in clinical practice.
-
Key words:
- children /
- allergic rhinitis /
- surgical treatment /
- radio frequency ablation /
- inferior turbinate
-

-
表 1 2组术前术后VAS评分比较
X ± S 症状 术前 术后 P 鼻塞 8.41±1.01 2.60±0.73 <0.05 打鼾 7.62±1.23 1.19±1.04 <0.05 口呼吸 6.33±1.12 3.55±1.60 <0.05 -
[1] Dykewicz MS, Wallace DV, Baroody F, et al. Treatment of seasonal allergic rhinitis: An evidence-based focused 2017 guideline update[J]. Ann Allergy Asthma Immunol, 2017, 119(6): 489-511. e41. doi: 10.1016/j.anai.2017.08.012
[2] Asher MI, Montefort S, Björkstén B, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys[J]. Lancet, 2006, 368(9537): 733-743. doi: 10.1016/S0140-6736(06)69283-0
[3] Kong WJ, Chen JJ, Zheng ZY, et al. Prevalence of allergic rhinitis in 3-6-year-old children in Wuhan of China[J]. Clin Exp Allergy, 2009, 39(6): 869-874. doi: 10.1111/j.1365-2222.2009.03206.x
[4] Milanesi JM, Berwig LC, Schuch LH, et al. Nasal patency and otorhinolaryngologic-orofacial features in children[J]. Braz J Otorhinolaryngol, 2019, 85(1): 83-91. doi: 10.1016/j.bjorl.2017.10.014
[5] Langille M, El-Hakim H. Pediatric inferior turbinoplasty with or without adenoidectomy: preliminary report on improvement of quality of life, symptom control, and safety[J]. J Otolaryngol Head Neck Surg, 2011, 40(5): 420-426.
[6] Seidman MD, Gurgel RK, Lin SY, et al. Clinical practice guideline: Allergic rhinitis[J]. Otolaryngol Head Neck Surg, 2015, 152(1 Suppl): S1-43.
[7] Valero A, Navarro AM, Del Cuvillo A, et al. Position paper on nasal obstruction: evaluation and treatment[J]. J Investig Allergol Clin Immunol, 2018, 28(2): 67-90. doi: 10.18176/jiaci.0232
[8] Hellings PW, Klimek L, Cingi C, et al. Non-allergic rhinitis: Position paper of the European Academy of Allergy and Clinical Immunology[J]. Allergy, 2017, 72(11): 1657-1665. doi: 10.1111/all.13200
[9] 章如新. 变应性鼻炎的外科治疗[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(1): 1-4. doi: 10.13201/j.issn.1001-1781.2020.01.001
[10] Kohlberg GD, Stewart MG, Ward RF, et al. Evaluation and management of pediatric nasal obstruction: A survey of practice patterns[J]. Am J Rhinol Allergy, 2016, 30(4): 274-278. doi: 10.2500/ajra.2016.30.4327
[11] Komshian SR, Cohen MB, Brook C, et al. Inferior Turbinate Hypertrophy: A Review of the Evolution of Management in Children[J]. Am J Rhinol Allergy, 2019, 33(2): 212-219. doi: 10.1177/1945892418815351
[12] 中华耳鼻咽喉头颈外科杂志编辑委员会鼻科组, 中华医学会耳鼻咽喉头颈外科学分会鼻科学组. 中国变应性鼻炎诊断和治疗指南(2022年, 修订版)[J]. 中华耳鼻咽喉头颈外科杂志, 2022, 57(2): 106-129. doi: 10.3760/cma.j.cn115330-20211228-00828
[13] Meltzer EO, Blaiss MS, Derebery MJ, et al. Burden of allergic rhinitis: results from the Pediatric Allergies in America survey[J]. J Allergy Clin Immunol, 2009, 124(3 Suppl): S43-70.
[14] Mallol J, Crane J, von Mutius E, et al. The International Study of Asthma and Allergies in Childhood(ISAAC)Phase Three: a global synthesis[J]. Allergol Immunopathol(Madr), 2013, 41(2): 73-85. doi: 10.1016/j.aller.2012.03.001
[15] Manzi B, Sykes KJ, Wei JL. Sinonasal Quality of Life in Children After Outfracture of Inferior Turbinates and Submucous Inferior Turbinoplasty for Chronic Nasal Congestion[J]. JAMA Otolaryngol Head Neck Surg, 2017, 143(5): 452-457. doi: 10.1001/jamaoto.2016.3889
[16] Chai G, Governale L, McMahon AW, et al. Trends of outpatient prescription drug utilization in US children, 2002-2010[J]. Pediatrics, 2012, 130(1): 23-31. doi: 10.1542/peds.2011-2879
[17] Cassano M, Maselli Del Giudice A, Russo G, et al. The role of nasal cytology in the management of inferior turbinate hypertrophy[J]. Int J Immunopathol Pharmacol, 2013, 26(1): 207-215. doi: 10.1177/039463201302600120
[18] Lin HC, Lin PW, Friedman M, et al. Long-term results of radiofrequency turbinoplasty for allergic rhinitis refractory to medical therapy[J]. Arch Otolaryngol Head Neck Surg, 2010, 136(9): 892-895. doi: 10.1001/archoto.2010.135
[19] Lee VS, Gold RM, Parikh SR. Short-term quality of life outcomes following pediatric septoplasty[J]. Acta Otolaryngol, 2017, 137(3): 293-296. doi: 10.1080/00016489.2016.1229023
[20] Wright AL, Holberg CJ, Martinez FD, et al. Epidemiology of physician-diagnosed allergic rhinitis in childhood[J]. Pediatrics, 1994, 94(6 Pt 1): 895-901.
[21] Segal S, Eviatar E, Berenholz L, et al. Inferior turbinectomy in children[J]. Am J Rhinol, 2003, 17(2): 69-73;discussion 69. doi: 10.1177/194589240301700201
[22] Gary CC. Pediatric nasal surgery: timing and technique[J]. Curr Opin Otolaryngol Head Neck Surg, 2017, 25(4): 286-290. doi: 10.1097/MOO.0000000000000378
[23] Cheng PW, Fang KM, Su HW, et al. Improved objective outcomes and quality of life after adenotonsillectomy with inferior turbinate reduction in pediatric obstructive sleep apnea with inferior turbinate hypertrophy[J]. Laryngoscope, 2012, 122(12): 2850-2854. doi: 10.1002/lary.23590
[24] Sullivan S, Li K, Guilleminault C. Nasal obstruction in children with sleep-disordered breathing[J]. Ann Acad Med Singap, 2008, 37(8): 645-648. doi: 10.47102/annals-acadmedsg.V37N8p645
[25] Chen YL, Tan CT, Huang HM. Long-term efficacy of microdebrider-assisted inferior turbinoplasty with lateralization for hypertrophic inferior turbinates in patients with perennial allergic rhinitis[J]. Laryngoscope, 2008, 118(7): 1270-1274. doi: 10.1097/MLG.0b013e31816d728e
[26] Pang YT, Willatt DJ. Laser reduction of inferior turbinates in children[J]. Singapore Med J, 1995, 36(5): 514-516.
[27] Calvo-Henriquez C, Capasso R, Martínez-Capoccioni G, et al. Safeness, subjective and objective changes after turbinate surgery in pediatric patients: A systematic review[J]. Int J Pediatr Otorhinolaryngol, 2020, 135: 110128. doi: 10.1016/j.ijporl.2020.110128
[28] Thompson AC. Surgical reduction of the inferior turbinate in children: extended follow-up[J]. J Laryngol Otol, 1989, 103(6): 577-579. doi: 10.1017/S0022215100109375
[29] Batra PS, Seiden AM, Smith TL. Surgical management of adult inferior turbinate hypertrophy: a systematic review of the evidence[J]. Laryngoscope, 2009, 119(9): 1819-1827. doi: 10.1002/lary.20544
[30] Arganbright JM, Jensen EL, Mattingly J, et al. Utility of Inferior Turbinoplasty for the Treatment of Nasal Obstruction in Children: A 10-Year Review[J]. JAMA Otolaryngol Head Neck Surg, 2015, 141(10): 901-904.
[31] Rejali SD, Upile T, McLellan D, et al. Inferior turbinate reduction in children using Holmium YAG laser-a clinical and histological study[J]. Lasers Surg Med, 2004, 34(4): 310-314. doi: 10.1002/lsm.20037
[32] Montgomery J, Sadiq H, Kubba H. Long-term follow-up of children after submucosal diathermy to the inferior turbinate for rhinitis[J]. Int J Pediatr Otorhinolaryngol, 2011, 75(3): 387-390. doi: 10.1016/j.ijporl.2010.12.013
[33] Lenz H, Eichler J, Knof J, et al. Endonasales Ar+-Laser-Strahlführungssystem und erste klinische Anwendungen bei der Rhinopathia vasomotorica[Endonasal Ar+-laser beam guide system and first clinical application in vasomotor rhinitis(author's transl)][J]. Laryngol Rhinol Otol(Stuttg), 1977, 56(9): 749-755.
[34] Araki S, Suzuki N, Sato H, et al. Endoscopic laser treatment for pediatric nasal allergy[J]. Diagn Ther Endosc, 2000, 6(4): 189-192. doi: 10.1155/DTE.6.189
[35] Chen YL, Liu CM, Huang HM. Comparison of microdebrider-assisted inferior turbinoplasty and submucosal resection for children with hypertrophic inferior turbinates[J]. Int J Pediatr Otorhinolaryngol, 2007, 71(6): 921-927. doi: 10.1016/j.ijporl.2007.03.002
[36] Bhattacharyya N, Kepnes LJ. Clinical effectiveness of coblation inferior turbinate reduction[J]. Otolaryngol Head Neck Surg, 2003, 129(4): 365-371. doi: 10.1016/S0194-59980300634-X
[37] O'Connor-Reina C, Garcia-Iriarte MT, Angel DG, et al. Radiofrequency volumetric tissue reduction for treatment of turbinate hypertrophy in children[J]. Int J Pediatr Otorhinolaryngol, 2007, 71(4): 597-601. doi: 10.1016/j.ijporl.2006.12.009
[38] Siméon R, Soufflet B, Souchal Delacour I. Coblation turbinate reduction in childhood allergic rhinitis[J]. Eur Ann Otorhinolaryngol Head Neck Dis, 2010, 127(2): 77-82. doi: 10.1016/j.anorl.2010.04.004
[39] Bitar MA, Kanaan AA, Sinno S. Efficacy and safety of inferior turbinates coblation in children[J]. J Laryngol Otol, 2014, 128 Suppl 2: S48-54.
[40] Jiang ZY, Pereira KD, Friedman NR, et al. Inferior turbinate surgery in children: a survey of practice patterns[J]. Laryngoscope, 2012, 122(7): 1620-1623. doi: 10.1002/lary.23292
[41] Yilmaz M, Kemalo lu YK, Baysal E, et al. Radiofrequency for inferior turbinate hypertrophy: could its long-term effect be predicted with a preoperative topical vasoconstrictor drop test?[J]. Am J Rhinol, 2006, 20(1): 32-35. doi: 10.1177/194589240602000106
[42] Leong SC, Kubba H, White PS. A review of outcomes following inferior turbinate reduction surgery in children for chronic nasal obstruction[J]. Int J Pediatr Otorhinolaryngol, 2010, 74(1): 1-6. doi: 10.1016/j.ijporl.2009.09.002
[43] Yuen SN, Leung PP, Funamura J, et al. Complications of turbinate reduction surgery in combination with tonsillectomy in pediatric patients[J]. Laryngoscope, 2017, 127(8): 1920-1923. doi: 10.1002/lary.26421
[44] Weider DJ, Sulzner SE. Inferior turbinate reduction surgery in children[J]. Ear Nose Throat J, 1998, 77(4): 304-306, 311-312, 314-315. doi: 10.1177/014556139807700413
[45] 钟建文, 罗向前, 仇书要, 等. 下鼻甲黏膜下等离子消融术对变应性鼻炎合并阻塞性睡眠呼吸暂停综合征患儿疗效及安全性初步研究[J]. 临床耳鼻咽喉头颈外科杂志, 2022, 36(10): 758-762. doi: 10.13201/j.issn.2096-7993.2022.10.006
-

计量
- 文章访问数: 72
- 施引文献: 0



 下载:
下载: