Risk factors of recurrence and canceration for premalignant vocal fold lesions after surgery
-
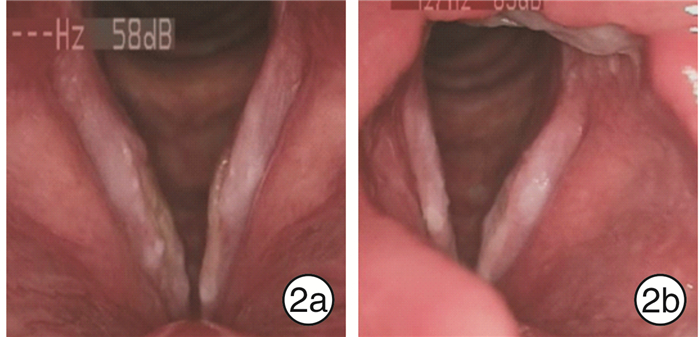
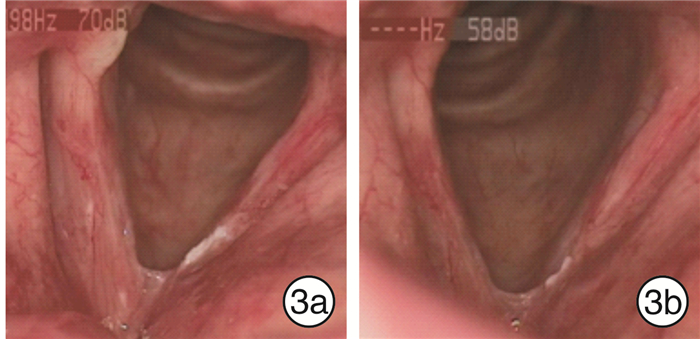
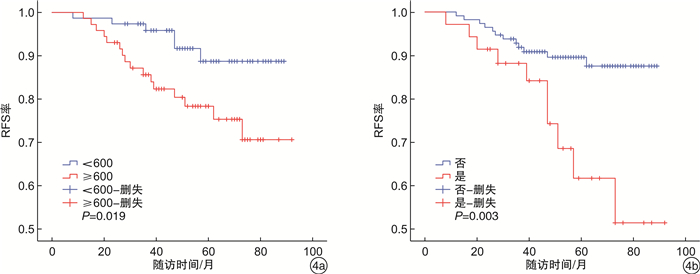
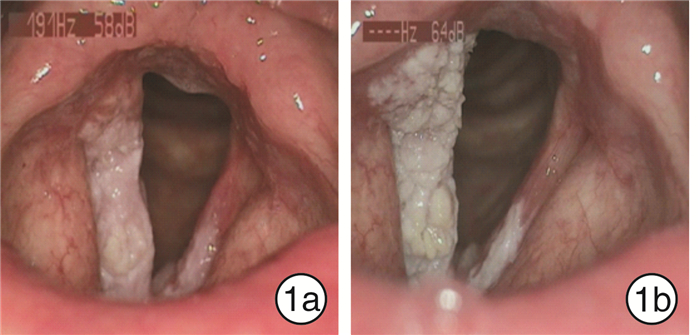
摘要: 目的 分析声带癌前病变术后复发和恶变的危险因素,为术前评估及术后随访提供合理依据。方法 回顾性分析2014-2017年在重庆市人民医院接受手术治疗的148例声带癌前病变患者临床病理因素与临床结局(复发、恶变、无复发生存率和无恶变生存率)之间的关系。结果 患者5年总复发率为14.86%,总恶变率为8.78%。单因素分析显示,吸烟指数、喉咽反流和病变范围与复发显著相关(P < 0.05),吸烟指数和病变范围与恶变显著相关(P < 0.05)。多因素logistic回归分析显示,吸烟指数≥600和喉咽反流是复发的独立危险因素(P < 0.05),吸烟指数≥600和病变范围≥1/2声带是恶变的独立危险因素(P < 0.05)。术后戒烟者的平均恶变间隔时间较未戒烟者明显更长(P < 0.05)。结论 过度吸烟、喉咽反流和病变范围≥1/2声带可能与声带癌前病变的术后复发或恶性进展有关,未来需要大规模的多中心前瞻性随机对照研究进一步明确上述影响因素对声带癌前病变术后复发和恶变的影响,以便制定更好的防范和治疗措施。Abstract: Objective To analyze the risk factors of recurrence and canceration for premalignant vocal fold lesions after surgery, and to provide a reasonable basis for preoperative evaluation and postoperative follow-up.Methods This study retrospective analyzed the relationship between clinicopathological factors and clinical outcome(recurrence, canceration, recurrence-free survival, and canceration-free survival) in 148 patients undergoing surgical treatment in Chongqing General Hospital from 2014 to 2017.Results The five-year overall recurrence rate was 14.86% and the overall recurrence rate was 8.78%. Univariate analysis showed that smoking index, laryngopharyngeal reflux and lesion range were significantly associated with recurrence(P < 0.05), and smoking index and lesion range were significantly associated with canceration(P < 0.05). Multivariate logistic regression analysis showed that smoking index ≥600 and laryngopharyngeal reflux were independent risk factors for recurrence(P < 0.05), and smoking index ≥600 and lesion range ≥1/2 vocal cord were independent risk factors for canceration(P < 0.05). The mean carcinogenesis interval for the postoperative smoking cessation group was significantly longer(P < 0.05).Conclusion Excessive smoking, laryngopharyngeal reflux and a wide range of lesions may be related to postoperative recurrence or malignant progression of precancerous lesions in the vocal cord, and further large-scale multi-center prospective randomized controlled studies are needed to clarify the effects of the above factors on recurrence and malignant changes in the future.
-

-
表 1 声带癌前病变患者术后复发与恶变相关临床病理特征
临床特征 例数 复发 恶变 例数(%) P 例数(%) P 性别 女 11 2(18.18) 1(9.09) 男 137 20(14.60) 1.000 12(8.76) 1.000 年龄/岁 < 65 68 13(19.12) 9(13.24) ≥65 80 9(11.25) 0.180 4(5.00) 0.078 饮酒 否 70 10(14.29) 4(5.89) 偶尔 43 5(11.63) 4(6.67) 长期 35 7(20.00) 0.576 5(14.29) 0.456 吸烟指数 < 600 76 6(7.89) 3(3.95) ≥600 72 16(22.22) 0.014 10(13.89) 0.033 喉咽反流 否 113 12(10.62) 9(7.96) 是 35 10(28.57) 0.010 4(11.43) 0.771 病变范围 < 1/2声带 108 12(11.11) 4(3.70) ≥1/2声带 40 10(25.00) 0.035 9(22.50) 0.001 前连合 否 98 13(13.27) 7(7.14) 是 50 9(18.00) 0.444 6(12.00) 0.496 厚度 薄 68 9(13.24) 6(8.82) 厚 80 13(16.25) 0.607 7(8.75) 0.994 表面 光滑 81 11(13.58) 6(7.41) 粗糙 67 11(16.42) 0.629 7(10.45) 0.515 充血 否 116 17(14.66) 9(7.76) 是 32 5(15.63) 1.000 4(12.50) 0.627 病理 低级别 71 9(12.68) 5(7.04) 高级别 77 13(16.88) 0.472 8(10.40) 0.472 表 2 多因素logistic回归分析
临床特征 复发 恶变 OR(95%CI) P OR(95%CI) P 性别(男vs女) 2.307(0.282~18.882) 0.436 0.803(0.048~13.483) 0.879 年龄(≥65岁vs < 65岁) 0.418(0.125~1.400) 0.157 0.571(0.121~2.700) 0.480 饮酒(偶尔vs否) 0.573(0.139~2.368) 0.442 1.160(0.179~7.517) 0.876 饮酒(长期vs否) 1.549(0.366~6.553) 0.552 2.229(0.356~13.943) 0.392 吸烟指数(≥600 vs < 600) 3.742(1.217~11.505) 0.021 5.369(1.108~26.011) 0.037 喉咽反流(是vs否) 6.465(1.661~25.168) 0.007 1.253(0.316~4.977) 0.517 病变范围(≥1/2声带vs < 1/2声带) 1.654(0.442~6.189) 0.455 6.547(1.267~33.820) 0.025 前连合(是vs否) 1.990(0.573~6.905) 0.278 1.094(0.244~4.905) 0.907 厚度(厚vs薄) 2.227(0.718~6.906) 0.165 0.941(0.221~4.010) 0.934 表面(粗糙vs光滑) 0.389(0.124~1.221) 0.106 0.323(0.074~1.403) 0.131 充血(是vs否) 2.284(0.596~8.757) 0.228 2.902(0.575~14.637) 0.197 病理(高级别vs低级别) 1.152(0.405~3.278) 0.792 1.600(0.389~6.574) 0.515 -
[1] Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[2] Hrelec C. Management of Laryngeal Dysplasia and Early Invasive Cancer[J]. Curr Treat Options Oncol, 2021, 22(10): 90. doi: 10.1007/s11864-021-00881-w
[3] Lim JY, Park YM, Kang M, et al. Angiolytic laser stripping versus CO2 laser microflap excision for vocal fold leukoplakia: Long-term disease control and voice outcomes[J]. PLoS One, 2018, 13(12): e0209691. doi: 10.1371/journal.pone.0209691
[4] Karatayli-Ozgursoy S, Pacheco-Lopez P, Hillel AT, et al. Laryngeal dysplasia, demographics, and treatment: a single-institution, 20-year review[J]. JAMA Otolaryngol Head Neck Surg, 2015, 141(4): 313-318. doi: 10.1001/jamaoto.2014.3736
[5] Sannino N, Mehlum CS, Grøntved ÅM, et al. Incidence and malignant transformation of glottic precursor lesions in Denmark[J]. Acta Oncol, 2020, 59(5): 596-602. doi: 10.1080/0284186X.2020.1730437
[6] Granda-Díaz R, Menéndez ST, Pedregal Mallo D, et al. The Novel Role of SOX2 as an Early Predictor of Cancer Risk in Patients with Laryngeal Precancerous Lesions[J]. Cancers(Basel), 2019, 11(3).
[7] Young CK, Lin WN, Lee LY, et al. Laryngoscopic characteristics in vocal leukoplakia: inter-rater reliability and correlation with histology grading[J]. Laryngoscope, 2015, 125(2): E62-66. doi: 10.1002/lary.24884
[8] Cho KJ, Song JS. Recent Changes of Classification for Squamous Intraepithelial Lesions of the Head and Neck[J]. Arch Pathol Lab Med, 2018, 142(7): 829-832. doi: 10.5858/arpa.2017-0438-RA
[9] Wu J, You K, Qiu X, et al. Age as Indicator in the Selection of Surgery Modalities in Early Glottic Cancer[J]. Risk Manag Healthc Policy, 2021, 14: 3223-3231. doi: 10.2147/RMHP.S317294
[10] van Hulst AM, Kroon W, van der Linden ES, et al. Grade of dysplasia and malignant transformation in adults with premalignant laryngeal lesions[J]. Head Neck, 2016, 38 Suppl 1: E2284-E2290.
[11] Tan C, Fang J, Wang R, et al. Risk factors for local recurrence of early bilateral vocal cord carcinoma treated with transoral CO2laser microsurgery[J]. Acta Otolaryngol, 2021, 141(9): 860-864. doi: 10.1080/00016489.2021.1925958
[12] Lee DH, Yoon TM, Lee JK, et al. Predictive factors of recurrence and malignant transformation in vocal cord leukoplakia[J]. Eur Arch Otorhinolaryngol, 2015, 272(7): 1719-1724. doi: 10.1007/s00405-015-3587-8
[13] Rzepakowska A, Marcinkiewicz B, urek M, et al. Motivation to smoking cessation in head and neck cancer and dysplasia patients in confrontation with the attitudes of otorhinolaryngologists in delivering anti-smoking therapies[J]. Eur Arch Otorhinolaryngol, 2022, 279(7): 3645-3655. doi: 10.1007/s00405-021-07209-2
[14] Zhang QW, Wang JY, Qiao XF, et al. Variations in disease burden of laryngeal cancer attributable to alcohol use and smoking in 204 countries or territories, 1990-2019[J]. BMC Cancer, 2021, 21(1): 1082. doi: 10.1186/s12885-021-08814-4
[15] Lechien JR, Mouawad F, Bobin F, et al. Review of management of laryngopharyngeal reflux disease[J]. Eur Ann Otorhinolaryngol Head Neck Dis, 2021, 138(4): 257-267. doi: 10.1016/j.anorl.2020.11.002
[16] Sasaki CT, Doukas SG, Doukas PG, et al. Weakly Acidic Bile Is a Risk Factor for Hypopharyngeal Carcinogenesis Evidenced by DNA Damage, Antiapoptotic Function, and Premalignant Dysplastic Lesions In Vivo[J]. Cancers(Basel), 2021, 13(4).
[17] Geterud A, Bove M, Ruth M. Hypopharyngeal acid exposure: an independent risk factor for laryngeal cancer?[J]. Laryngoscope, 2003, 113(12): 2201-2205. doi: 10.1097/00005537-200312000-00030
[18] Tae K, Jin BJ, Ji YB, et al. The role of laryngopharyngeal reflux as a risk factor in laryngeal cancer: a preliminary report[J]. Clin Exp Otorhinolaryngol, 2011, 4(2): 101-104. doi: 10.3342/ceo.2011.4.2.101
[19] Rodrigo JP, Villaronga MÁ, Menéndez ST, et al. A Novel Role For Nanog As An Early Cancer Risk Marker In Patients With Laryngeal Precancerous Lesions[J]. Sci Rep, 2017, 7(1): 11110. doi: 10.1038/s41598-017-11709-9
[20] Manterola L, Aguirre P, Larrea E, et al. Mutational profiling can identify laryngeal dysplasia at risk of progression to invasive carcinoma[J]. Sci Rep, 2018, 8(1): 6613. doi: 10.1038/s41598-018-24780-7
[21] Baran CA, Agaimy A, Wehrhan F, et al. MAGE-A expression in oral and laryngeal leukoplakia predicts malignant transformation[J]. Mod Pathol, 2019, 32(8): 1068-1081. doi: 10.1038/s41379-019-0253-5
[22] Yang SW, Lee YS, Chang LC, et al. Oral tongue leukoplakia: analysis of clinicopathological characteristics, treatment outcomes, and factors related to recurrence and malignant transformation[J]. Clin Oral Investig, 2021, 25(6): 4045-4058. doi: 10.1007/s00784-020-03735-1
-



 下载:
下载: