Development and validation of nomogram for predicting prognosis of patients with laryngeal squamous cell carcinoma after surgery
-
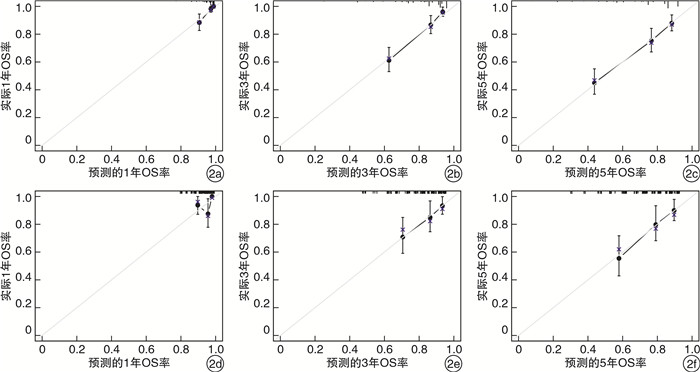
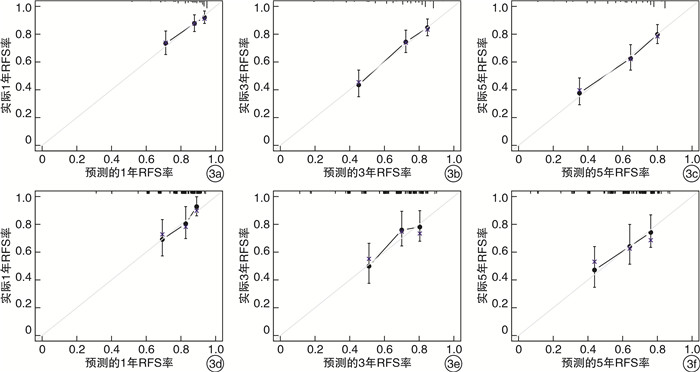
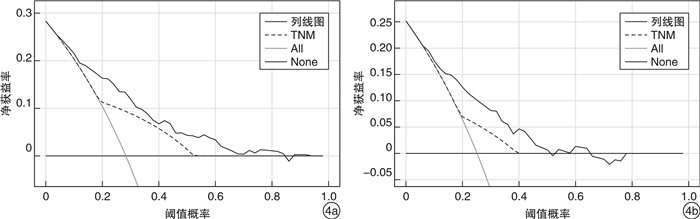
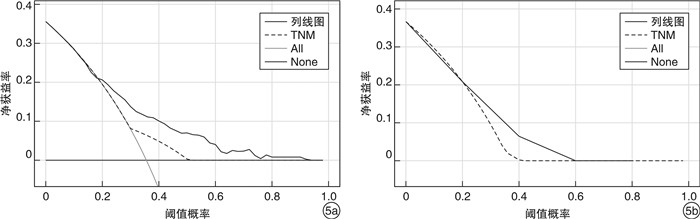
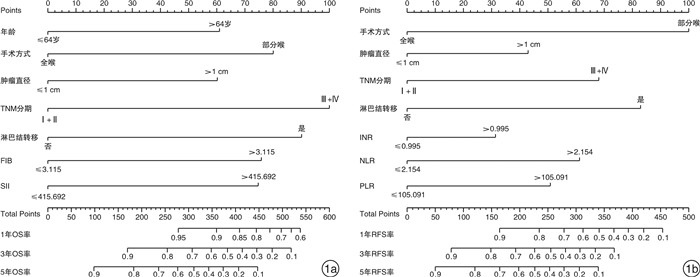
摘要: 目的 探讨术前血液功能指标、临床病理特征与喉鳞状细胞癌(LSCC)术后患者预后的关系,建立LSCC患者术后生存和复发时间的预测列线图。方法 回顾性分析接受初次手术治疗的530例LSCC患者的病例资料。将患者按7∶3的比例随机分为训练组(371例)和验证组(159例),基于Cox回归模型构建总生存期(OS)和无复发生存期(RFS)列线图,对列线图进行验证,并与肿瘤TNM分期进行比较。结果 多因素分析结果显示年龄、手术方式、肿瘤直径、TNM分期、颈部淋巴结转移、纤维蛋白原水平和系统免疫炎症指数与OS显著相关,手术方式、肿瘤直径、TNM分期、颈部淋巴结转移、国际标准化比值、中性粒细胞与淋巴细胞比值、血小板与淋巴细胞比值与RFS显著相关。基于上述因素构建列线图,训练组OS及RFS列线图的C-index分别为0.755和0.687,均高于TNM分期(0.657和0.582);验证组OS及RFS列线图的C-index分别为0.717和0.646,均高于TNM分期(0.599和0.528)。本列线图的受试者工作特征曲线下面积也均高于TNM分期。校准曲线显示模型具有较好的一致性。决策曲线分析显示本列线图比TNM分期具有更高的临床获益。结论 基于独立预后因素构建的LSCC术后患者的1、3、5年OS和RFS的预测列线图,该模型对指导LSCC个体化诊疗有一定的临床意义。Abstract: Objective To explore the relationship between preoperative blood indexes, clinicopathological characteristics and prognosis of patients with laryngeal squamous cell carcinoma(LSCC), and to establish a nomogram for predicting survival and recurrence time of LSCC patients.Methods The clinical data of 530 patients with LSCC who received primary surgical treatment were analyzed retrospectively. The patients were randomly divided into training group and testing group according to the ratio of 7∶3. The nomograms of overall survival(OS) and recurrence-free survival(RFS) were constructed based on Cox regression model, and the nomograms were verified and compared with TNM stage.Results The results of multivariate analysis showed that age, operation mode, tumor diameter, TNM stage, cervical lymph node metastasis, fibrinogen level and systemic immune inflammation index were significantly correlated with OS, while operation mode, tumor diameter, TNM stage, cervical lymph node metastasis, international normalized ratio, neutrophil to lymphocyte ratio and platelet to lymphocyte ratio were significantly correlated with RFS. The nomograms were constructed based on the above factors. The C-indexes of the nomograms of OS and RFS in the training group were 0.755 and 0.687, respectively, which were higher than those of TNM stage(0.657 and 0.582). In the testing group, the C-indexes of OS and RFS nomograms were 0.717 and 0.646, respectively, which were higher than those of TNM stage(0.599 and 0.528). The area under the receiver operating characteristic curves of these nomograms were also higher than TNM stage. The calibration curves showed that the models had good consistency. Decision curve analysis(DCA) showed that these nomograms had higher clinical benefit than TNM stage.Conclusion Based on the independent prognostic factors, the predictive nomograms of OS and RFS at 1, 3 and 5 years after LSCC were constructed, which have certain clinical significance in guiding the individualized diagnosis and treatment of LSCC.
-
Key words:
- laryngeal neoplasms /
- carcinoma, squamous cell /
- overall survival /
- recurrence-free survival /
- prognosis /
- nomogram
-

-
表 1 LSCC患者的临床特征
例(%) 项目 总例数(n=530) 训练组(n=371) 验证组(n=159) P值 年龄/岁 1.000 ≤64 287(54.2) 195(52.6) 92(57.9) >64 243(45.8) 176(47.4) 67(42.1) 性别 1.000 男 514(97.0) 362(97.6) 152(95.6) 女 16(3.0) 9(2.4) 7(4.4) 手术方式 1.000 部分喉a) 394(74.3) 275(74.1) 119(74.8) 全喉b) 136(25.7) 96(25.9) 40(25.2) 肿瘤部位 1.000 声门型 414(78.1) 286(77.1) 128(80.5) 非声门型 116(21.9) 85(22.9) 31(19.5) 肿瘤最大直径/cm 1.000 ≤1 274(51.7) 191(51.5) 83(52.2) >1 256(48.3) 180(48.5) 76(47.8) TNM分期 1.000 Ⅰ+Ⅱ 381(71.9) 268(72.2) 113(71.1) Ⅲ+Ⅳ 149(28.1) 103(27.8) 46(28.9) 病理分化程度 1.000 高+中 461(87.0) 326(87.9) 135(84.9) 低 69(13.0) 45(12.1) 24(15.1) 颈部淋巴结转移 0.931 否 464(87.5) 324(87.3) 140(88.1) 是 66(12.5) 47(12.7) 19(11.9) 咽瘘 0.750 否 506(95.5) 353(95.1) 153(96.2) 是 24(4.5) 18(4.9) 6(3.8) 注:a)部分喉包括各种形式的经口支撑喉镜下手术及开放式喉部分切除术;b)全喉即全喉切除术。 表 2 训练组中OS的单因素和多因素Cox回归分析
项目 单因素 多因素 HR(95%CI) P值 HR(95%CI) P值 年龄/岁(≤64 vs. >64) 1.716(1.161~2.537) 0.007 1.695(1.135~2.532) 0.010 性别(男vs.女) 0.415(0.058~2.972) 0.381 手术方式(部分喉vs.全喉) 2.776(1.887~4.084) <0.001 0.445(0.219~0.907) 0.026 肿瘤部位(声门型vs.非声门型) 2.571(1.736~3.807) <0.001 肿瘤直径/cm(≤1 vs. >1) 2.830(1.873~4.274) <0.001 1.691(1.010~2.831) 0.046 TNM分期(Ⅰ+Ⅱvs.Ⅲ+Ⅳ) 3.677(2.505~5.396) <0.001 2.429(1.212~4.867) 0.012 病理分化程度(高+中vs.低) 2.539(1.598~4.034) <0.001 颈部淋巴结转移(否vs.是) 3.909(2.544~6.005) <0.001 2.069(1.143~3.745) 0.016 咽瘘(否vs.是) 2.356(1.189~4.668) 0.014 FIB(≤3.115 vs. >3.115) 3.178(2.146~4.705) <0.001 1.967(1.290~3.000) 0.002 SII(≤415.692 vs. >415.692) 2.649(1.802~3.895) <0.001 1.913(1.270~2.881) 0.002 表 3 训练组中RFS的单因素和多因素Cox回归分析
项目 单因素 多因素 HR(95%CI) P值 HR(95%CI) P值 年龄/岁(≤64 vs. >64) 1.227(0.872~1.726) 0.242 性别(男vs.女) 0.826(0.263~2.596) 0.744 手术方式(部分喉vs.全喉) 1.584(1.100~2.280) 0.014 0.285(0.139~0.584) < 0.001 肿瘤部位(声门型vs.非声门型) 1.910(1.327~2.751) < 0.001 肿瘤直径/cm(≤1 vs. >1) 1.991(1.404~2.824) < 0.001 1.591(1.030~2.456) 0.036 TNM分期(Ⅰ+Ⅱvs.Ⅲ+Ⅳ) 2.064(1.454~2.929) < 0.001 2.035(1.003~4.128) 0.049 病理分化程度(高+中vs.低) 1.784(1.128~2.821) 0.013 颈部淋巴结转移(否vs.是) 2.631(1.740~3.977) < 0.001 2.072(1.124~3.822) 0.020 咽瘘(否vs.是) 1.899(0.996~3.620) 0.052 INR(≤0.995 vs. >0.995) 1.550(1.097~2.189) 0.013 1.450(1.018~2.065) 0.039 NLR(≤2.154 vs. >2.154) 2.378(1.689~3.349) < 0.001 1.627(1.005~2.636) 0.048 dNLR(≤1.344 vs. >1.344) 1.728(1.223~2.442) 0.002 PLR(≤105.091 vs. >105.091) 2.376(1.682~3.357) < 0.001 1.524(1.005~2.312) 0.048 MLR(≤0.234 vs. >0.234) 2.058(1.452~2.917) < 0.001 SII(≤405.968 vs. >405.968) 2.491(1.765~3.515) <0.001 -
[1] Yang Z, Jin J, Chang T. CircPTK2(hsa_circ_0003221) Contributes to Laryngeal Squamous Cell Carcinoma by the miR-1278/YAP1 Axis[J]. J Oncol, 2021, 2021: 2408384.
[2] 龚洪立, 周梁, 陶磊, 等. 局部晚期声门型喉癌的肿瘤体积对患者生存率的影响[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(4): 316-320. doi: 10.13201/j.issn.2096-7993.2021.04.007
[3] Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries[J]. CA Cancer J Clin, 2021, 71(3): 209-249. doi: 10.3322/caac.21660
[4] Iasonos A, Schrag D, Raj GV, et al. How to build and interpret a nomogram for cancer prognosis[J]. J Clin Oncol, 2008, 26(8): 1364-1370. doi: 10.1200/JCO.2007.12.9791
[5] Abdol Razak NB, Jones G, Bhandari M, et al. Cancer-Associated Thrombosis: An Overview of Mechanisms, Risk Factors, and Treatment[J]. Cancers(Basel), 2018, 10(10): 380.
[6] Singh N, Baby D, Rajguru JP, et al. Inflammation and cancer[J]. Ann Afr Med, 2019, 18(3): 121-126. doi: 10.4103/aam.aam_56_18
[7] Gundog M, Basaran H. Pretreatment low prognostic nutritional index and low albumin-globulin ratio are predictive for overall survival in nasopharyngeal cancer[J]. Eur Arch Otorhinolaryngol, 2019, 276(11): 3221-3230. doi: 10.1007/s00405-019-05595-2
[8] Zhang L, Ye J, Luo Q, et al. Prediction of Poor Outcomes in Patients with Colorectal Cancer: Elevated Preoperative Prothrombin Time(PT)and Activated Partial Thromboplastin Time(APTT)[J]. Cancer Manag Res, 2020, 12: 5373-5384. doi: 10.2147/CMAR.S246695
[9] López JA. Introduction to a review series on platelets and cancer[J]. Blood, 2021, 137(23): 3151-3152. doi: 10.1182/blood.2020010237
[10] Bauckneht M, Rebuzzi SE, Signori A, et al. The prognostic power of inflammatory indices and clinical factors in metastatic castration-resistant prostate cancer patients treated with radium-223(BIO-Ra study)[J]. Eur J Nucl Med Mol Imaging, 2022, 49(3): 1063-1074. doi: 10.1007/s00259-021-05550-6
[11] Cho U, Park HS, Im SY, et al. Prognostic value of systemic inflammatory markers and development of a nomogram in breast cancer[J]. PLoS One, 2018, 13(7): e0200936. doi: 10.1371/journal.pone.0200936
[12] Xiong S, Dong L, Cheng L. Neutrophils in cancer carcinogenesis and metastasis[J]. J Hematol Oncol, 2021, 14(1): 173. doi: 10.1186/s13045-021-01187-y
[13] Liu C, Wang W, Meng X, et al. Albumin/globulin ratio is negatively correlated with PD-1 and CD25 mRNA levels in breast cancer patients[J]. Onco Targets Ther, 2018, 11: 2131-2139. doi: 10.2147/OTT.S159481
[14] Okadome K, Baba Y, Yagi T, et al. Prognostic Nutritional Index, Tumor-infiltrating Lymphocytes, and Prognosis in Patients with Esophageal Cancer[J]. Ann Surg, 2020, 271(4): 693-700. doi: 10.1097/SLA.0000000000002985
[15] Cai H, Zhang ZH, Zhou YJ, et al. The Prognostic Value of Preoperative Plasma Fibrinogen and Neutrophil-to-Lymphocyte Ratio in Patients With Laryngeal Squamous Cell Carcinoma[J]. Ear Nose Throat J, 2021, 100(10): 731-736. doi: 10.1177/0145561320920746
[16] Woodley N, Rogers ADG, Turnbull K, et al. Prognostic scores in laryngeal cancer[J]. Eur Arch Otorhinolaryngol, 2022, 279(7): 3705-3715. doi: 10.1007/s00405-021-07233-2
[17] Li Z, Qu Y, Yang Y, et al. Prognostic value of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio and systemic immune-inflammation index in patients with laryngeal squamous cell carcinoma[J]. Clin Otolaryngol, 2021, 46(2): 395-405. doi: 10.1111/coa.13689
[18] 陈玉莲, 李运明, 秦杨, 等. 晚期非小细胞肺癌患者凝血功能异常的相关因素与预后的分析[J]. 中国医学前沿杂志(电子版), 2017, 9(3): 41-45. https://www.cnki.com.cn/Article/CJFDTOTAL-YXQY201703010.htm
[19] Amin MB, Greene FL, Edge SB, et al. The Eighth Edition AJCC Cancer Staging Manual: Continuing to build a bridge from a population-based to a more "personalized" approach to cancer staging[J]. CA Cancer J Clin, 2017, 67(2): 93-99. doi: 10.3322/caac.21388
[20] Balachandran VP, Gonen M, Smith JJ, et al. Nomograms in oncology: more than meets the eye[J]. Lancet Oncol, 2015, 16(4): e173-80. doi: 10.1016/S1470-2045(14)71116-7
[21] 胡晨, 薛继尧, 龚洪立, 等. 喉鳞状细胞癌局部复发影响因素及预后分析[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(9): 773-776. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202009002.htm
[22] Cui J, Wen Q, Tan X, et al. A Genomic-Clinicopathologic Nomogram Predicts Survival for Patients with Laryngeal Squamous Cell Carcinoma[J]. Dis Markers, 2019, 2019: 5980567.
[23] Cui J, Wang L, Zhong W, et al. Development and validation of nomogram to predict risk of survival in patients with laryngeal squamous cell carcinoma[J]. Biosci Rep, 2020, 40(8).
-




 下载:
下载: