Current status of the diagnosis and treatment of temporal bone squamous cell carcinoma
-
摘要: 颞骨鳞状细胞癌是颞骨恶性肿瘤中最常见的类型,临床罕见。该病的罕见性导致其分期、颞骨的切除方法、腮腺和颈部淋巴结的处理以及放化疗的应用等仍然存在诸多争议,国内外至今未提出针对性指南共识。本文对颞骨鳞状细胞癌诊断与治疗的最新进展进行综述,希望能够对该病的诊疗提供一定的帮助和参考。Abstract: Temporal bone squamous cell carcinoma, which is rare in the clinical setting, is the most common type of temporal bone malignancy. Its rarity makes the staging, the way of temporal bone resection, the management of parotid gland and cervical lymph node, and the application of radiotherapy and chemotherapy still controversial.There is no unanimous consensus and guideline about it to date at home and abroad.This paper reviewed the recent advance in the diagnosis and treatment of temporal bone squamous cell carcinoma in the hope of providing some help and reference for the management of the disease.
-
Key words:
- temporal bone /
- squamous cell carcinoma /
- diagnosis /
- treatment
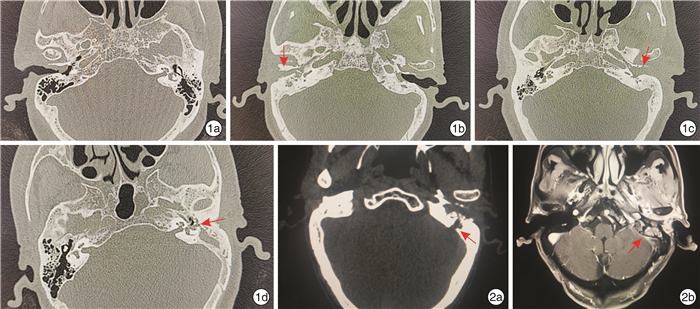
-

-
表 1 改良匹兹堡分期标准
分期 具体描述 T分期 T1 肿瘤局限于外耳道,不伴骨质破坏或软组织累及 T2 肿瘤局限于外耳道,伴有骨质破坏(未及全层)或者有局限性(< 0.5 cm)软组织累及 T3 肿瘤侵及骨性外耳道(累及全层)且软组织受累有限(< 0.5 cm)或者肿瘤侵及中耳和/或乳突 T4 肿瘤侵及耳蜗、岩尖、中耳内壁、颈动脉管、颈静脉孔或硬脑膜,或广泛性(>0.5 cm)软组织累及,如侵及颞下颌关节或茎突,或伴有面神经麻痹的证据 N分期 N0 无区域淋巴结转移 N1 同侧单个淋巴结转移,直径≤3 cm,且ENE(-) N2a 同侧单个淋巴结转移,直径>3~6 cm,且ENE(-) N2b 同侧多个淋巴结转移,直径≤6 cm,且ENE(-) N2c 双侧或对侧淋巴结转移,最大直径≤6 cm,且ENE(-) N3a 最大直径>6 cm且ENE(-)的淋巴结转移 N3b 任何表现为临床ENE(+)的淋巴结转移 总体分期 Ⅰ期 T1N0M0 Ⅱ期 T2N0M0 Ⅲ期 T3N0M0 Ⅳ期 T4N0M0,任何T1~4N+M0,任何T1~4N0M1,任何T1~4N+M1 ENE:淋巴结包膜外播散。 -
[1] Lechner M, Sutton L, Murkin C, et al. Squamous cell cancer of the temporal bone: a review of the literature[J]. Eur Arch Otorhinolaryngol, 2021, 278(7): 2225-2228. doi: 10.1007/s00405-020-06281-4
[2] Seligman KL, Sun DQ, Ten Eyck PP, et al. Temporal bone carcinoma: Treatment patterns and survival[J]. Laryngoscope, 2020, 130(1): E11-E20.
[3] Piras G, Grinblat G, Albertini R, et al. Management of squamous cell carcinoma of the temporal bone: long-term results and factors influencing outcomes[J]. Eur Arch Otorhinolaryngol, 2021, 278(9): 3193-3202. doi: 10.1007/s00405-020-06378-w
[4] Snietura M, Chelmecka-Wiktorczyk L, Pakulo S, et al. Vertically transmitted HPV-dependent squamous cell carcinoma of the external auditory canal: Case report of a child[J]. Strahlenther Onkol, 2017, 193(2): 156-161. doi: 10.1007/s00066-016-1047-z
[5] Sato K, Komune N, Hongo T, et al. Genetic landscape of external auditory canal squamous cell carcinoma[J]. Cancer Sci, 2020, 111(8): 3010-3019. doi: 10.1111/cas.14515
[6] Allanson BM, Low TH, Clark JR, et al. Squamous Cell Carcinoma of the External Auditory Canal and Temporal Bone: An Update[J]. Head Neck Pathol, 2018, 12(3): 407-418. doi: 10.1007/s12105-018-0908-4
[7] De Roeck L, Nuyts S. Bilateral radiation-induced squamous cell carcinomas of the external auditory canal 30 years after radiotherapy for a pituitary adenoma: a case report[J]. Tumori, 2019, 105(6): NP4-NP7. doi: 10.1177/0300891619832258
[8] Liu H, Zhang Y, Zhang T, et al. Correlation between the pathology and clinical presentations in patients with adenoid cystic carcinoma of the external auditory canal[J]. Head Neck, 2017, 39(12): 2444-2449. doi: 10.1002/hed.24915
[9] Wang Z, Zheng M, Xia S. The contribution of CT and MRI in staging, treatment planning and prognosis prediction of malignant tumors of external auditory canal[J]. Clin Imaging, 2016, 40(6): 1262-1268. doi: 10.1016/j.clinimag.2016.08.020
[10] Kiyokawa Y, Ariizumi Y, Ohno K, et al. Indications for and extent of elective neck dissection for lymph node metastasis from external auditory canal carcinoma[J]. Auris Nasus Larynx, 2021, 48(4): 745-750. doi: 10.1016/j.anl.2020.12.002
[11] Kim SY, Beer M, Tshering Vogel DW. Imaging in head and neck cancers: Update for non-radiologist[J]. Oral Oncol, 2021, 120: 105434. doi: 10.1016/j.oraloncology.2021.105434
[12] Razek A. Assessment of Masses of the External Ear With Diffusion-Weighted MR Imaging[J]. Otol Neurotol, 2018, 39(2): 227-231. doi: 10.1097/MAO.0000000000001629
[13] Beyea JA, Moberly AC. Squamous cell carcinoma of the temporal bone[J]. Otolaryngol Clin North Am, 2015, 48(2): 281-292. doi: 10.1016/j.otc.2014.12.003
[14] Nader ME, Ginsberg LE, Bell D, et al. Evaluating Perineural Spread to the Intratemporal Facial Nerve on Magnetic Resonance Imaging[J]. Otolaryngol Head Neck Surg, 2019, 160(6): 1087-1094. doi: 10.1177/0194599819827848
[15] Xie B, Zhang T, Dai C. Survival outcomes of patients with temporal bone squamous cell carcinoma with different invasion patterns[J]. Head Neck, 2015, 37(2): 188-196. doi: 10.1002/hed.23576
[16] Toriihara A, Nakadate M, Fujioka T, et al. Clinical Usefulness of 18F-FDG PET/CT for Staging Cancer of the External Auditory Canal[J]. Otol Neurotol, 2018, 39(5): e370-e375. doi: 10.1097/MAO.0000000000001791
[17] Moody SA, Hirsch BE, Myers EN. Squamous cell carcinoma of the external auditory canal: an evaluation of a staging system[J]. Am J Otol, 2000, 21(4): 582-588.
[18] Nabuurs CH, Kievit W, Labbé N, et al. Evaluation of the modified Pittsburgh classification for predicting the disease-free survival outcome of squamous cell carcinoma of the external auditory canal[J]. Head Neck, 2020, 42(12): 3609-3622. doi: 10.1002/hed.26424
[19] Zanoletti E, Franz L, Cazzador D, et al. Temporal bone carcinoma: Novel prognostic score based on clinical and histological features[J]. Head Neck, 2020, 42(12): 3693-3701. doi: 10.1002/hed.26435
[20] Franz L, Zanoletti E, Franchella S, et al. Temporal bone carcinoma: testing the prognostic value of a novel clinical and histological scoring system[J]. Eur Arch Otorhinolaryngol, 2021, 278(11): 4179-4186. doi: 10.1007/s00405-020-06489-4
[21] Muelleman T, Chowdhury NI, Killeen D, et al. Effect of Piecemeal vs En Bloc Approaches to the Lateral Temporal Bone on Survival Outcomes[J]. Otolaryngol Head Neck Surg, 2018, 158(4): 716-720. doi: 10.1177/0194599818758994
[22] Matoba T, Hanai N, Suzuki H, et al. Treatment and Outcomes of Carcinoma of the External and Middle Ear: The Validity of En Bloc Resection for Advanced Tumor[J]. Neurol Med Chir(Tokyo), 2018, 58(1): 32-38. doi: 10.2176/nmc.oa.2017-0133
[23] Mehta GU, Muelleman TJ, Brackmann DE, et al. Temporal bone resection for lateral skull-base malignancies[J]. J Neurooncol, 2020, 150(3): 437-444. doi: 10.1007/s11060-020-03445-4
[24] Gidley PW, DeMonte F. Lateral Temporal Bone Resection[M]. Cham Switzerland: Springer International Publishing, 2018: 229-243.
[25] Mazzoni A, Zanoletti E, Marioni G, et al. En bloc temporal bone resections in squamous cell carcinoma of the ear. Technique, principles, and limits[J]. Acta Otolaryngol, 2016, 136(5): 425-432. doi: 10.3109/00016489.2015.1126352
[26] Rindler RS, Soriano RM, Elsherbini MM, et al. Exoscopic En Bloc Carotid-Sparing Total Temporal Bone Resection: Feasibility Study and Operative Technique[J]. World Neurosurg, 2022, 160: e1-e8. doi: 10.1016/j.wneu.2021.08.115
[27] Omura G, Ando M, Saito Y, et al. Survival impact of local extension sites in surgically treated patients with temporal bone squamous cell carcinoma[J]. Int J Clin Oncol, 2017, 22(3): 431-437. doi: 10.1007/s10147-016-1076-8
[28] Prasad SC, D'Orazio F, Medina M, et al. State of the art in temporal bone malignancies[J]. Curr Opin Otolaryngol Head Neck Surg, 2014, 22(2): 154-165. doi: 10.1097/MOO.0000000000000035
[29] Lovin BD, Gidley PW. Squamous cell carcinoma of the temporal bone: A current review[J]. Laryngoscope Investig Otolaryngol, 2019, 4(6): 684-692. doi: 10.1002/lio2.330
[30] Zhang T, Li W, Dai C, et al. Evidence-based surgical management of T1 or T2 temporal bone malignancies[J]. Laryngoscope, 2013, 123(1): 244-248. doi: 10.1002/lary.23637
[31] Homer JJ, Lesser T, Moffat D, et al. Management of lateral skull base cancer: United Kingdom National Multidisciplinary Guidelines[J]. J Laryngol Otol, 2016, 130(S2): S119-S124. doi: 10.1017/S0022215116000542
[32] Morita S, Homma A, Nakamaru Y, et al. The Outcomes of Surgery and Chemoradiotherapy for Temporal Bone Cancer[J]. Otol Neurotol, 2016, 37(8): 1174-1182. doi: 10.1097/MAO.0000000000001152
[33] Xie B, Wang M, Zhang S, et al. Parotidectomy in the management of squamous cell carcinoma of the external auditory canal[J]. Eur Arch Otorhinolaryngol, 2021, 278(5): 1355-1364. doi: 10.1007/s00405-020-06191-5
[34] Lee JM, Joo JW, Kim SH, et al. Evidence Based Tailored Parotidectomy in Treating External Auditory Canal Carcinoma[J]. Sci Rep, 2018, 8(1): 12112. doi: 10.1038/s41598-018-30536-0
[35] 韩宇, 李瑞, 杨润琴, 等. 早期外耳道癌的临床特点及预后相关因素分析[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(10): 874-879. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202110003.htm
[36] Zanoletti E, Mazzoni A, Martini A, et al. Surgery of the lateral skull base: a 50-year endeavour[J]. Acta Otorhinolaryngol Ital, 2019, 39(SUPPL. 1): S1-S146.
[37] Vozel D, Pukl P, Groselj A, et al. The importance of flaps in reconstruction of locoregionally advanced lateral skull-base cancer defects: a tertiary otorhinolaryngology referral centre experience[J]. Radiol Oncol, 2021, 55(3): 323-332. doi: 10.2478/raon-2021-0012
[38] Parr JM, Chouhan P, Wagels M. Anterolateral thigh versus pectoralis major flaps in reconstruction of the lateral temporal bone defect[J]. ANZ J Surg, 2019, 89(4): E132-E136. doi: 10.1111/ans.14922
[39] Trojanowski P, Szymański M, Trojanowska A, et al. Anterolateral thigh free flap in reconstruction of lateral skull base defects after oncological resection[J]. Eur Arch Otorhinolaryngol, 2019, 276(12): 3487-3494. doi: 10.1007/s00405-019-05627-x
[40] Bertelsen C, Simsolo E, Maceri D, et al. Outcomes of reconstruction after temporal bone resection for malignancy[J]. J Craniomaxillofac Surg, 2018, 46(10): 1856-1861. doi: 10.1016/j.jcms.2018.08.002
[41] Bi X, Liu B, Mao Z, et al. Applications of materials for dural reconstruction in pre-clinical and clinical studies: Advantages and drawbacks, efficacy, and selections[J]. Mater Sci Eng C Mater Biol Appl, 2020, 117: 111326. doi: 10.1016/j.msec.2020.111326
[42] Shinomiya H, Uehara N, Teshima M, et al. Clinical management for T1 and T2 external auditory canal cancer[J]. Auris Nasus Larynx, 2019, 46(5): 785-789. doi: 10.1016/j.anl.2019.02.004
[43] Zhong S, Zuo W. Treatment Strategies for Malignancies of the External Auditory Canal[J]. Curr Treat Options Oncol, 2022, 23(1): 43-53. doi: 10.1007/s11864-021-00931-3
[44] Pemberton LS, Swindell R, Sykes AJ. Primary radical radiotherapy for squamous cell carcinoma of the middle ear and external auditory cana--an historical series[J]. Clin Oncol(R Coll Radiol), 2006, 18(5): 390-394. doi: 10.1016/j.clon.2006.03.001
[45] Ogawa K, Nakamura K, Hatano K, et al. Treatment and prognosis of squamous cell carcinoma of the external auditory canal and middle ear: a multi-institutional retrospective review of 87 patients[J]. Int J Radiat Oncol Biol Phys, 2007, 68(5): 1326-1334. doi: 10.1016/j.ijrobp.2007.01.052
[46] Koto M, Hasegawa A, Takagi R, et al. Carbon ion radiotherapy for locally advanced squamous cell carcinoma of the external auditory canal and middle ear[J]. Head Neck, 2016, 38(4): 512-516. doi: 10.1002/hed.23905
[47] Shiga K, Nibu KI, Fujimoto Y, et al. Multi-institutional Survey of Squamous Cell Carcinoma of the External Auditory Canal in Japan[J]. Laryngoscope, 2021, 131(3): E870-E874.
[48] Fujiwara M, Yamamoto S, DoiH, et al. Arterial chemoradiotherapy for carcinomas of the external auditory canal and middle ear[J]. Laryngoscope, 2015, 125(3): 685-689. doi: 10.1002/lary.24908
[49] Takenaka Y, Cho H, Nakahara S, et al. Chemoradiation therapy for squamous cell carcinoma of the external auditory canal: A meta-analysis[J]. Head Neck, 2015, 37(7): 1073-1080. doi: 10.1002/hed.23698
[50] Komune N, Noda T, Kogo R, et al. Primary Advanced Squamous Cell Carcinoma of the Temporal Bone: A Single-Center Clinical Study[J]. Laryngoscope, 2021, 131(2): E583-E589.
[51] Zanoletti E, Marioni G, Franchella S, et al. Recurrent squamous cell carcinoma of the temporal bone: critical analysis of cases with a poor prognosis[J]. Am J Otolaryngol, 2015, 36(3): 352-355. doi: 10.1016/j.amjoto.2014.12.008
[52] Park JM, Kong JS, Chang KH, et al. The Clinical Characteristics and Surgical Outcomes of Carcinoma of the External Auditory Canal: A Multicenter Study[J]. J Int Adv Otol, 2018, 14(2): 278-284. doi: 10.5152/iao.2018.4952
[53] George M, Borsotti F, Gereige R, et al. A systematic review of the primary squamous cell carcinoma of the external auditory canal: survival outcome based on T-staging and proposal of a new classification[J]. J Laryngol Otol, 2021, 135(2): 96-103. doi: 10.1017/S0022215121000323
[54] Shiga K, Nibu KI, Fujimoto Y, et al. Sites of invasion of cancer of the external auditory canal predicting oncologic outcomes[J]. Head Neck, 2021, 43(10): 3097-3105. doi: 10.1002/hed.26800
[55] Komune N, Miyazaki M, Sato K, et al. Prognostic Impact of Tumor Extension in Patients With Advanced Temporal Bone Squamous Cell Carcinoma[J]. Front Oncol, 2020, 10: 1229. doi: 10.3389/fonc.2020.01229
[56] McCracken M, Pai K, Cabrera CI, et al. Temporal Bone Resection for Squamous Cell Carcinoma of the Lateral Skull Base: Systematic Review and Meta-analysis[J]. Otolaryngol Head Neck Surg, 2022: 1945998221084912.
[57] Hongo T, Kuga R, Miyazaki M, et al. Programmed Death-Ligand 1 Expression and Tumor-Infiltrating Lymphocytes in Temporal Bone Squamous Cell Carcinoma[J]. Laryngoscope, 2021, 131(12): 2674-2683. doi: 10.1002/lary.29689
[58] Miyazaki M, Aoki M, Okado Y, et al. Highly expressed tumoral emmprin and stromal CD73 predict a poor prognosis for external auditory canal carcinoma[J]. Cancer Sci, 2020, 111(8): 3045-3056. doi: 10.1111/cas.14508
[59] Komune N, Sato K, Hongo T, et al. Prognostic Significance of Systemic Inflammatory Response in Cases of Temporal Bone Squamous Cell Carcinoma[J]. Laryngoscope, 2021, 131(8): 1782-1789. doi: 10.1002/lary.29421
-




 下载:
下载: