Association of sudden sensorineural hearing loss and its prognosis with the brain white matter hyperintensity
-
摘要: 目的 探讨脑白质高信号(WMH)与突发性聋(简称突聋)的关系及对突聋预后的影响。方法 纳入2019年6月—2020年6月期间以单侧突聋住院的患者50例(突聋组)和年龄、性别匹配无突聋病史的常规体检者50例(对照组)进行病例对照研究。所有纳入对象完善3.0T头颅磁共振检查,采用Fazekas量表对脑室周围白质高信号(PVWMH)和深部白质高信号(DWMH)进行独立评分,比较突聋组与对照组Fazekas评分和Fazekas评分频率分布情况,采用有序logistic回归研究突聋患者预后与WMH的关系。结果 突聋患者WMH的Fazekas评分明显高于对照组(PVWMH:P=0.004,DWMH:P=0.010);突聋组与对照组Fazekas评分频率分布差异有统计学意义(PVWMH:P=0.036,DWMH:P=0.047);有序logistic回归结果显示突聋患者不合并WMH即Fazekas=0是突聋预后良好的独立预测因素(P=0.025,OR=12.779)。结论 突聋患者合并脑白质高信号较无突聋者更常见,不合并脑白质高信号较合并脑白质高信号的突聋患者预后更好。Abstract: Objective To explore the relationship between white matter hyperintensity(WMH) and sudden sensorineural hearing loss(SSHL) and evaluate the influence of WMH on the prognosis of SSHL.Methods Fifty hospitalized unilateral SSHL patients and 50 age and gender matched routine physical examination individuals without SSHL history from June 2019 to June 2020 were included for a case-control study. All included subjects underwent 3.0 Tesla cranial magnetic resonance examination, and the Fazekas scale was applied to evaluate periventricular white matter hyperintense(PVWMH) and deep white matter hyperintense(DWMH). Fazekas score and distribution proportions of Fazekas score was compared between SSHL and control. Ordered logistic regression was used to study the relationship between prognosis of SSHL and WMH.Results The Fazekas score of WMH in SSHL group was significantly higher than that of control group(PVWMH: P=0.004, DWMH: P=0.010); There was a significant difference in the distribution proportions of Fazekas scores between SSHL and control(PVWMH: P=0.036, DWMH: P=0.047); The results of ordered logistic regression showed that patients without WMH(Fazekas=0) is an independent predictor of good prognosis in SSHL(P=0.025, OR=12.779).Conclusion The prevalence of WMH in SSHL patients was higher than that of control. SSHL patients without WMH has a better prognosis than those with WMH.
-
突发性聋(简称突聋)的病因、病理生理机制不完全明确,可能的发病机制有血栓栓塞及微血栓形成、内听动脉痉挛、膜迷路积水及毛细胞损失等[1]。糖皮质激素联合改善内耳循环药物对各型突聋均有改善作用[2],但影响突聋预后的因素繁杂且结论各有差异[3-4]。脑白质疏松(leukoaraiosis)在磁共振T2加权成像(T2WI)和液体衰减反转恢复序列(fluid-attenuated inversion recovery,FLAIR)成像为高信号白色亮点,故又称作脑白质高信号(white matter hyperintense,WMH)或脑白质病变[5]。已有研究提示WMH与卒中、认知功能障碍、运动及步态障碍、情感障碍等相关[6-7],但WMH与突聋的关系研究目前尚无明确结论。本文旨在研究WMH和突聋的关系,探讨WMH对突聋预后的影响。
1. 资料与方法
1.1 研究对象及分组
收集2019年6月—2020年6月在宝鸡市中心医院诊断为单侧突聋并住院治疗的50例患者为突聋组。纳入标准:符合《突发性聋诊断和治疗指南(2015)》[8]的诊断标准; 年龄大于18岁; 单侧发病; 无激素使用禁忌; 有完整听力学检查资料; 所有突聋患者均根据指南给予标准化治疗。排除标准:既往有梅尼埃病、中耳炎、乳突炎及外伤、药物毒性等明确原因所致听力损害; 听力学检查及病例资料不完善。收集同期年龄、性别匹配的50例体检者作为对照组,所有体检者均否认突聋病史及听力减退相关主诉,均完成头颅磁共振(MRI)检查。
1.2 头颅MRI检查及Fazekas评分
MRI检查采用GE Discovery MR 750W 3.0T静音MR系统完成头颅扫描,扫描序列包括T1WI、T2WI、T2 FLAIR。采用Fazekas量表对脑室周围白质高信号(periventricular white matter hyperintense,PVWMH)和深部白质高信号(deep white matter hyperintense,DWMH)进行独立评分(表 1),Fazekas评分=0为无WMH,≥1为存在WMH。由2名经验丰富的神经科医师对头颅MRI结果进行Fazekas评分,若存在分歧则由影像科MRI医师复核判定,经讨论后最终评分。
表 1 脑白质病变Fazekas评分病变部位 0分 1分 2分 3分 PVWMH 脑室旁无病灶 帽状或者铅笔样薄层病变 光滑的光晕病变 病变延伸到深部白质 DWMH 脑深部无病变 点状高信号 开始融合的点状病灶 大面积融合的病灶 1.3 听力检查及疗效评估
突聋患者于入院时、治疗7 d及治疗1个月后检查纯音测听阈值。根据世界卫生组织标准,以500、1000、2000、4000 Hz平均听阈将听力损失分为轻度(平均听阈26~40 dB HL)、中度(平均听阈41~60 dB HL)、重度(平均听阈61~80 dB HL)、极重度(平均听阈≥81 dB HL)。按照《突发性聋诊断和治疗指南(2015)》[8]评估预后:听力恢复正常、达发病前水平或健侧耳水平为痊愈,受损频率听力平均提高大于30 dB为显效,15~30 dB为有效,小于15 dB为无效。
1.4 治疗方法
根据指南[8]所有突聋患者均口服醋酸泼尼松片1 mg/kg,最大用量60 mg,每日1次,连用5 d,金纳多87.5~105 mg静脉滴注,平坦下降型和全聋型加用巴曲酶治疗,首次剂量10 BU,之后每次5 BU,隔日使用1次,共5次,使用期间检测凝血功能。
1.5 统计学方法
应用SPSS 23.0统计软件分析数据,计数资料以个数及百分比表示,组间比较采用χ2检验; 计量资料行正态分布性检验,符合正态分布以X±S表示,组间比较采用独立样本t检验; 不符合正态分布以中位数(四分位数)表示,组间比较采用Mann-Whitney U检验; 突聋组和对照组Fazekas评分分布频率比较采用Fisher精确检验。以突聋预后为因变量,构建有序logistic回归模型研究WMH及其他因素对突聋预后的影响。P < 0.05为差异有统计学意义。
2. 结果
2.1 突聋组与对照组基线资料及WMH比较
突聋组与对照组基线资料及WMH比较见表 2。突聋组与对照组的年龄、性别差异无统计学意义(P>0.05),高血压、糖尿病以及甘油三酯、胆固醇、低密度脂蛋白的差异无统计学意义(P>0.05);两组PVWMH的Fazekas评分的差异有统计学意义(P=0.004),DWMH的Fazekas评分的差异有统计学意义(P=0.010)。
表 2 突聋组与对照组基线资料及WMH比较项目 突聋组(n=50) 对照组(n=50) t/Z/χ2 P值 年龄/岁 56.68±12.03 55.94±14.69 0.275 0.784 性别/例(%) 男性 24(48.0) 26(52.0) 0.360 0.548 女性 26(52.0) 24(48.0) 高血压/例(%) 19(38.0) 21(42.0) 0.167 0.683 糖尿病/例(%) 9(18.0) 10(20.0) 0.065 0.799 甘油三酯/(mmol·L-1) 1.44±0.61 1.57±0.82 -0.966 0.336 胆固醇/(mmol·L-1) 3.91±0.93 3.94±1.00 -1.560 0.876 低密度脂蛋白/(mmol·L-1) 2.85±1.23 3.03±1.01 -0.931 0.354 脑白质病变 PVWMH 1.02±0.14
1.0(0,3.0)0.50±0.10
0(0,2.0)-2.872 0.004 DWMH 0.94±0.13
1.0(0,3.0)0.48±0.10
0(0,2.0)-2.567 0.010 2.2 突聋组与对照组Fazekas评分分布频率比较
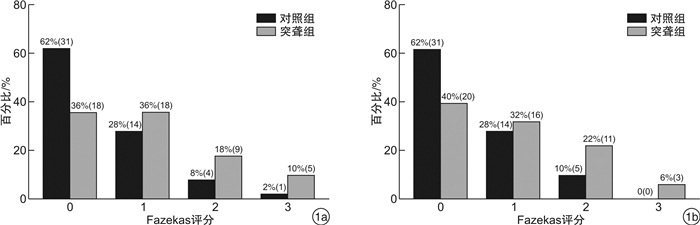
突聋组与对照组PVWMH的Fazekas评分分布频率差异有统计学意义(χ2=8.277,P=0.036),DWMH的Fazekas评分分布频率差异有统计学意义(χ2=7.296,P=0.047),见图 1。
2.3 突聋患者预后有序logistic回归分析结果
以突聋患者预后(赋值:1=无效,2=有效,3=显效,4=痊愈)为因变量Y,将可能影响预后的因素(年龄、性别、眩晕、耳鸣、发病时听力损失情况、听阈曲线类型、发病至治疗时间、高血压、糖尿病、血脂、WMH等)纳入模型进行多元有序logistic回归分析,具体变量因素及赋值见表 3。有序logistic回归结果提示:年龄小于60岁(P=0.036,OR=7.744),发病时轻度听力损失(P=0.028,OR= 37.675),发病至治疗时间小于3 d(P=0.047,OR=37.412),听阈曲线为低频下降型(P=0.003,OR=26.708)、平坦下降型(P=0.017,OR=17.921)是突聋预后良好的预测因素; 突聋合并眩晕者预后较差(P=0.042,OR=0.020),突聋患者不合并WMH即Fazekas=0是突聋预后良好的独立预测因素(P=0.025,OR=12.779)。结果详见表 4。
表 3 突聋组患者临床特征及变量赋值变量 例数(%) 变量及赋值 变量 例数(%) 变量及赋值 年龄/岁 56.68±12.03 X1 发病至治疗时间/d X6 <60 15(30) 1 1~3 11(22) 60~80 25(50) 2 4~14 23(46) >80 10(20) 3 >14 16(32) 性别 X2 听阈曲线类型 X7 男 24(48) 1 低频下降型 12(24) 女 26(52) 2 高频下降型 14(28) 合并眩晕 13(26) X3,1=眩晕,2=不眩晕 平坦下降型 13(26) 合并耳鸣 15(30) X4,1=耳鸣,2=不耳鸣 全聋型 11(22) 发病时听力损失程度 X5 脑血管危险因素 轻度 19(38) 1 高血压 19(38) X8,1=高血压,2=正常 中度 10(20) 2 糖尿病 9(18) X9,1=糖尿病,2=正常 重度 12(24) 3 高脂血症 20(40) X10,1=高脂血症,2=正常 极重度 9(18) 4 脑白质病变 X11 听力恢复情况 Y Fazekas=0 18(36) 1 无效 22(44) 1 Fazekas≥1 32(64) 2 有效 9(18) 2 显效 11(22) 3 痊愈 8(16) 4 表 4 突聋组患者预后有序Logistic回归分析结果影响因素 回归系数 标准误 Wald χ2 P值 OR(95%CI) 年龄/岁 <60 2.047 1.106 4.313 0.036 7.744(1.986~36.479) 60~80 1.353 0.812 1.237 0.401 3.869(1.684~22.463) >80(Ref) - - - - - 性别 男 -1.654 0.565 1.146 0.384 0.191(-1.174~4.363) 女(Ref) - - - - - 合并疾病 眩晕,X3=1 -3.909 1.013 4.144 0.042 0.020(-4.864~0.840) 耳鸣,X4=1 -0.596 0.457 0.167 0.682 0.551(-1.899~3.445) 发病听力损失程度 轻度 3.629 1.493 4.954 0.028 37.675(7.896~82.774) 中度 1.534 1.197 0.262 0.609 4.636(2.771~29.858) 重度 -0.901 0.961 0.273 0.601 0.406(-2.327~24.633) 极重度(Ref) - - - - - 发病至治疗时间/d 1~3 3.622 1.236 4.095 0.047 37.412(14.896~62.747) 4~14 1.501 1.285 0.238 0.505 4.486(2.882~32.737) >14(Ref) - - - - - 听阈曲线类型 低频下降型 3.258 1.136 8.693 0.003 26.708(7.896~82.774) 平坦下降型 2.886 1.196 5.658 0.017 17.921(4.896~52.101) 高频下降型 1.210 0.904 2.376 0.123 3.353(1.896~24.149) 全聋型(Ref) - - - - - 重度(Ref) - - - - - 高血压,X6=1 -0.755 0.735 3.075 0.080 0.947(0.224~3.996) 糖尿病,X7=1 -0.996 1.138 0.742 0.389 0.927(0.107~8.060) 高脂血症,X8=1 -0.930 0.701 1.287 0.257 0.379(0.070~2.050) WMH Fazekas=0 2.345 0.939 5.021 0.025 12.779(2.244~21.934) Fazekas≥1(Ref) - - - - - 3. 讨论
目前关于WMH与突聋关系的研究较少,且得出的结论存在差异。Dicuonzo等[9]研究发现突聋患者大多合并脑白质病变,但Ciorba等[10]提出突聋患者与对照人群发生脑白质病变的比例一致,两组无明显差异,但WMH与突聋患者听力恢复程度有关。本研究发现与对照组相比突聋患者更易合并WMH,无论是脑室周围(P=0.004)还是脑深部白质(P=0.010),突聋组Fazekas评分均较对照组高; Fazekas评分分布频率结果提示突聋组Fazekas评分≥1分的百分率明显高于对照组(图 1),综上表明突聋和WMH可能有密切关系,突聋组脑白质病变较对照组更严重。流行病学及临床研究提示突聋与脑血管危险因素及血流变学障碍有关[11]。内耳的血液供应主要来源于内听动脉,而内听动脉是小脑前下动脉主要分支,因此后循环缺血或内听动脉血栓梗死事件会导致听力损失及眩晕。也有研究发现突聋对缺血性卒中有预测作用[12]。WMH是脑小血管病的一种最常见亚型,是脑微循环障碍标志之一,WMH与脑卒中的发生和预后有密切关系,WMH越严重,脑梗死神经功能康复越差[13]。尽管突聋和WMH发病具体机制不明确,但两者均与小血管病变、缺血改变密切相关,因此可推测缺血/缺氧、血管调节所致低灌注、血管内皮损失以及炎症因子释放、氧化应激等因素共同参与突聋患者的WMH改变[14]。
突聋预后是否与年龄、听力损失程度、耳鸣、眩晕等相关仍存在争议[15],糖尿病、高血压、高脂血症等血管危险因素对突聋预后的研究结论不一致[16]。因此本研究选取年龄、眩晕、耳鸣、发病听力损失程度、听阈曲线类型、发病至治疗时间、高血压、糖尿病、高脂血症、WMH等探讨影响突聋的预后因素。与施紫光等(2010)研究一致,我们发现年龄对突聋预后有影响,随年龄增大,突聋预后逐渐变差,以60岁为节点,logistic结果提示小于60岁是突聋预后良好的预测因素(P=0.036,OR=7.744),可能原因是老年患者血管功能减退,合并多脑血管病危险因素多、机体修复功能减退。本研究发现3 d内治疗的突聋患者预后明显优于14 d以后治疗者(P=0.047,OR=37.412),潜在原因是支配内耳血供的迷路动脉缺乏侧支循环,初期毛细胞功能损害为可逆性,经积极治疗可完全恢复,随缺血时间延迟,毛细胞损害程度范围增加并出现不可逆损害,即使改善内耳缺血血氧其功能仍难以完全恢复[17]。我们发现WMH与突聋预后有密切关系,合并WMH的突聋患者即Fazekas≥1是突聋预后不佳的独立预测因素(P=0.025,OR=12.779)。轻度听力损失较中、重、极重度听力损失预后好(P=0.028,OR=37.675),这与Schreiber等(2010)研究结果相符,我们推测其潜在原因是不同听力损失程度反映耳蜗受损的程度,重度和极重度听力损失可能已产生不可逆性损害,药物治疗效果差。突聋患者听力损失同时伴有前庭功能障碍,合并眩晕可能是突聋预后不良的影响因素[18]。本研究发现合并眩晕是突聋预后不良的预测因素(P=0.042,OR=0.020),潜在原因是眩晕为后循环缺血典型症状,可以反映耳蜗和前庭的迷路供血障碍。有研究提出血糖、血压、血脂及代谢性因素对突聋预后有影响[16, 19],但本研究发现糖尿病、高血压、高脂血症、耳鸣等因素与突聋预后关系不大,可能因为本研究为回顾性研究,样本量较少。
综上,本研究发现突聋患者中WMH更常见,WMH可作为突聋预后不佳的独立预测因素。本研究存在不足:为单中心回顾性研究,样本量较小,结果可能存在偏倚,因此仍需大样本、多中心的前瞻性研究进一步证实。
利益冲突 所有作者均声明不存在利益冲突
-
表 1 脑白质病变Fazekas评分
病变部位 0分 1分 2分 3分 PVWMH 脑室旁无病灶 帽状或者铅笔样薄层病变 光滑的光晕病变 病变延伸到深部白质 DWMH 脑深部无病变 点状高信号 开始融合的点状病灶 大面积融合的病灶 表 2 突聋组与对照组基线资料及WMH比较
项目 突聋组(n=50) 对照组(n=50) t/Z/χ2 P值 年龄/岁 56.68±12.03 55.94±14.69 0.275 0.784 性别/例(%) 男性 24(48.0) 26(52.0) 0.360 0.548 女性 26(52.0) 24(48.0) 高血压/例(%) 19(38.0) 21(42.0) 0.167 0.683 糖尿病/例(%) 9(18.0) 10(20.0) 0.065 0.799 甘油三酯/(mmol·L-1) 1.44±0.61 1.57±0.82 -0.966 0.336 胆固醇/(mmol·L-1) 3.91±0.93 3.94±1.00 -1.560 0.876 低密度脂蛋白/(mmol·L-1) 2.85±1.23 3.03±1.01 -0.931 0.354 脑白质病变 PVWMH 1.02±0.14
1.0(0,3.0)0.50±0.10
0(0,2.0)-2.872 0.004 DWMH 0.94±0.13
1.0(0,3.0)0.48±0.10
0(0,2.0)-2.567 0.010 表 3 突聋组患者临床特征及变量赋值
变量 例数(%) 变量及赋值 变量 例数(%) 变量及赋值 年龄/岁 56.68±12.03 X1 发病至治疗时间/d X6 <60 15(30) 1 1~3 11(22) 60~80 25(50) 2 4~14 23(46) >80 10(20) 3 >14 16(32) 性别 X2 听阈曲线类型 X7 男 24(48) 1 低频下降型 12(24) 女 26(52) 2 高频下降型 14(28) 合并眩晕 13(26) X3,1=眩晕,2=不眩晕 平坦下降型 13(26) 合并耳鸣 15(30) X4,1=耳鸣,2=不耳鸣 全聋型 11(22) 发病时听力损失程度 X5 脑血管危险因素 轻度 19(38) 1 高血压 19(38) X8,1=高血压,2=正常 中度 10(20) 2 糖尿病 9(18) X9,1=糖尿病,2=正常 重度 12(24) 3 高脂血症 20(40) X10,1=高脂血症,2=正常 极重度 9(18) 4 脑白质病变 X11 听力恢复情况 Y Fazekas=0 18(36) 1 无效 22(44) 1 Fazekas≥1 32(64) 2 有效 9(18) 2 显效 11(22) 3 痊愈 8(16) 4 表 4 突聋组患者预后有序Logistic回归分析结果
影响因素 回归系数 标准误 Wald χ2 P值 OR(95%CI) 年龄/岁 <60 2.047 1.106 4.313 0.036 7.744(1.986~36.479) 60~80 1.353 0.812 1.237 0.401 3.869(1.684~22.463) >80(Ref) - - - - - 性别 男 -1.654 0.565 1.146 0.384 0.191(-1.174~4.363) 女(Ref) - - - - - 合并疾病 眩晕,X3=1 -3.909 1.013 4.144 0.042 0.020(-4.864~0.840) 耳鸣,X4=1 -0.596 0.457 0.167 0.682 0.551(-1.899~3.445) 发病听力损失程度 轻度 3.629 1.493 4.954 0.028 37.675(7.896~82.774) 中度 1.534 1.197 0.262 0.609 4.636(2.771~29.858) 重度 -0.901 0.961 0.273 0.601 0.406(-2.327~24.633) 极重度(Ref) - - - - - 发病至治疗时间/d 1~3 3.622 1.236 4.095 0.047 37.412(14.896~62.747) 4~14 1.501 1.285 0.238 0.505 4.486(2.882~32.737) >14(Ref) - - - - - 听阈曲线类型 低频下降型 3.258 1.136 8.693 0.003 26.708(7.896~82.774) 平坦下降型 2.886 1.196 5.658 0.017 17.921(4.896~52.101) 高频下降型 1.210 0.904 2.376 0.123 3.353(1.896~24.149) 全聋型(Ref) - - - - - 重度(Ref) - - - - - 高血压,X6=1 -0.755 0.735 3.075 0.080 0.947(0.224~3.996) 糖尿病,X7=1 -0.996 1.138 0.742 0.389 0.927(0.107~8.060) 高脂血症,X8=1 -0.930 0.701 1.287 0.257 0.379(0.070~2.050) WMH Fazekas=0 2.345 0.939 5.021 0.025 12.779(2.244~21.934) Fazekas≥1(Ref) - - - - - -
[1] Chandrasekhar SS, Tsai Do BS, Schwartz SR, et al. Clinical Practice Guideline: Sudden Hearing Loss(Update)[J]. Otolaryngol Head Neck Surg, 2019, 161(1_suppl): S1-S45. doi: 10.1177/0194599819859885
[2] 李佳, 王佳宁, 苏雅静, 等. 高剂量激素对突发性聋的挽救性治疗分析[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(7): 643-646. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202007017.htm
[3] Choo OS, Yang SM, Park HY, et al. Differences in clinical characteristics and prognosis of sudden low-and high-frequency hearing loss[J]. Laryngoscope, 2017, 127(8): 1878-1884. doi: 10.1002/lary.26382
[4] 钱怡, 钟时勋, 胡国华, 等. 突发性耳聋的分型治疗及预后分析[J]. 重庆医科大学学报, 2015, 40(8): 1159-1163. https://www.cnki.com.cn/Article/CJFDTOTAL-ZQYK201508020.htm
[5] Yuan J, Feng L, Hu W, et al. Use of Multimodal Magnetic Resonance Imaging Techniques to Explore Cognitive Impairment in Leukoaraiosis[J]. Med Sci Monit, 2018, 24: 8910-8915. doi: 10.12659/MSM.912153
[6] Dickie DA, Gardner K, Wagener A, et al. Cortical thickness, white matter hyperintensities, and cognition after stroke[J]. Int J Stroke, 2020, 15(1): 46-54. doi: 10.1177/1747493019851291
[7] Linortner P, McDaniel C, Shahid M, et al. White Matter Hyperintensities Related to Parkinson's Disease Executive Function[J]. Mov Disord Clin Pract, 2020, 7(6): 629-638. doi: 10.1002/mdc3.12956
[8] 中华耳鼻咽喉头颈外科杂志编辑委员会, 中华医学会耳鼻咽喉头颈外科学分会. 突发性聋诊断和治疗指南(2015)[J]. 中华耳鼻咽喉头颈外科杂志, 2015, 50(6): 443-447. doi: 10.3760/cma.j.issn.1673-0860.2015.06.002
[9] Dicuonzo F, Purciariello S, De Marco A, et al. MR evaluation of encephalic leukoaraiosis in sudden sensorineural hearing loss(SSNHL)patients[J]. Neurol Sci, 2019, 40(2): 357-362. doi: 10.1007/s10072-018-3647-0
[10] Ciorba A, Bianchini C, Crema L, et al. White matter lesions and sudden sensorineural hearing loss[J]. J Clin Neurosci, 2019, 65: 6-10. doi: 10.1016/j.jocn.2019.04.037
[11] Kim SY, Lim JS, Sim S, et al. Sudden Sensorineural Hearing Loss Predicts Ischemic Stroke: a Longitudinal Follow-Up Study[J]. Otol Neurotol, 2018, 39(8): 964-969. doi: 10.1097/MAO.0000000000001902
[12] Lammers M, Young E, Westerberg BD, et al. Risk of Stroke and Myocardial Infarction After Sudden Sensorineural Hearing Loss: A Meta-Analysis[J]. Laryngoscope, 2021, 131(6): 1369-1377. doi: 10.1002/lary.29237
[13] Luijten S, Bos D, Compagne K, et al. Association of White Matter Lesions and Outcome After Endovascular Stroke Treatment[J]. Neurology, 2021, 96(3): e333-e342. doi: 10.1212/WNL.0000000000010994
[14] Hainsworth AH, Minett T, Andoh J, et al. Neuropathology of White Matter Lesions, Blood-Brain Barrier Dysfunction, and Dementia[J]. Stroke, 2017, 48(10): 2799-2804. doi: 10.1161/STROKEAHA.117.018101
[15] Sciancalepore PI, de Robertis V, Sardone R, et al. Sudden sensorineural hearing loss: What factors influence the response to therapy?[J]. Audiol Res, 2020, 10(1): 234. doi: 10.4081/audiores.2020.234
[16] Kim JY, Hong JY, Kim DK. Association of Sudden Sensorineural Hearing Loss With Risk of Cardiocerebrovascular Disease: A Study Using Data From the Korea National Health Insurance Service[J]. JAMA Otolaryngol Head Neck Surg, 2018, 144(2): 129-135. doi: 10.1001/jamaoto.2017.2569
[17] Haremza C, Klopp-Dutote N, Strunski V, et al. Evaluation of cardiovascular risks and recovery of idiopathic sudden sensorineural hearing loss in hospitalised patients: comparison between complete and partial sudden sensorineural hearing loss[J]. J Laryngol Otol, 2017, 131(10): 919-924. doi: 10.1017/S0022215117001736
[18] 曹海南, 宋玲玲, 蒋雯, 等. 继发于突发性聋的良性阵发性位置性眩晕的疗效分析[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(3): 234-237. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202103009.htm
[19] Lin CF, Lee KJ, Yu SS, et al. Effect of comorbid diabetes and hypercholesterolemia on the prognosis of idiopathic sudden sensorineural hearing loss[J]. Laryngoscope, 2016, 126(1): 142-149. doi: 10.1002/lary.25333
期刊类型引用(3)
1. 朱斌,陈晨,张柳燕,关兵,徐丽. 不同预后的全聋型突发性聋患者治疗前失匹配负波的探讨. 听力学及言语疾病杂志. 2024(05): 437-440 .  百度学术
百度学术
2. 刘丹,刘逸远,张肖. 针刺联合高压氧中西医综合治疗突聋的疗效分析. 神经损伤与功能重建. 2024(11): 644-647 .  百度学术
百度学术
3. 李浩然,石宝洋,朱利利,刘勇,高明,付胜奇. 脑小血管病与突发性感音神经性聋的相关性. 国际脑血管病杂志. 2023(06): 429-434 .  百度学术
百度学术
其他类型引用(2)
-




 DownLoad:
DownLoad: