Risk and prognostic analysis of cervical lymph node metastasis in cN+ laryngeal squamous cell carcinoma
-
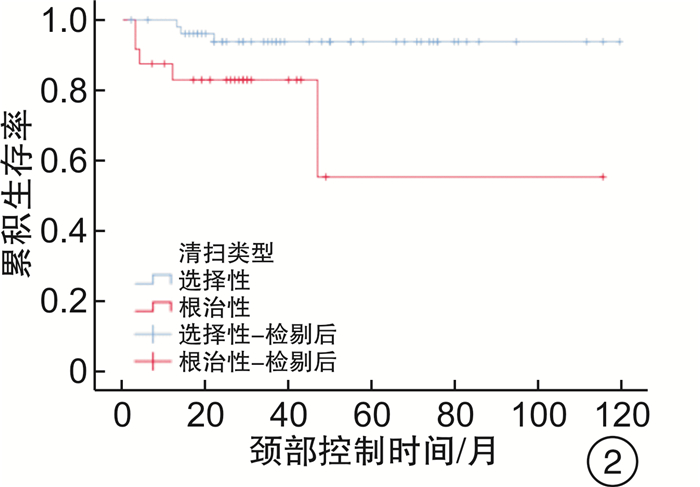
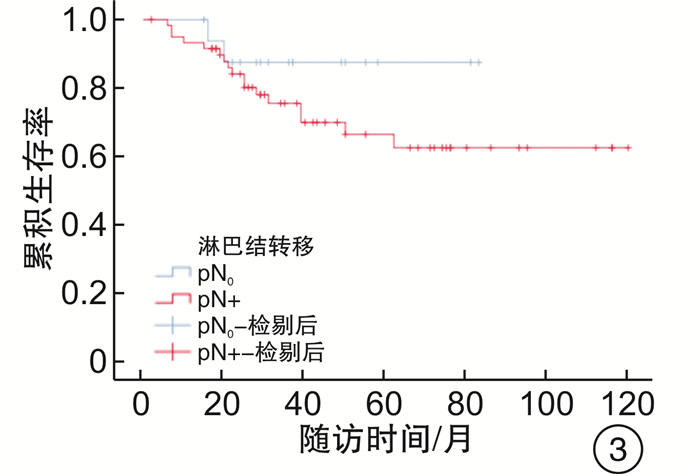
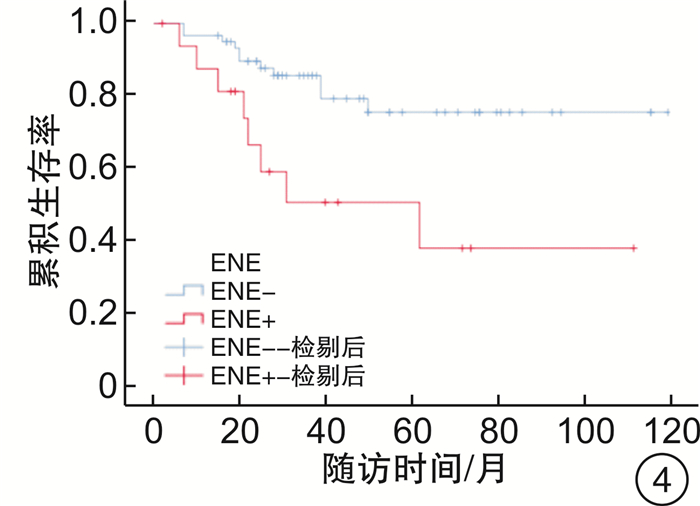
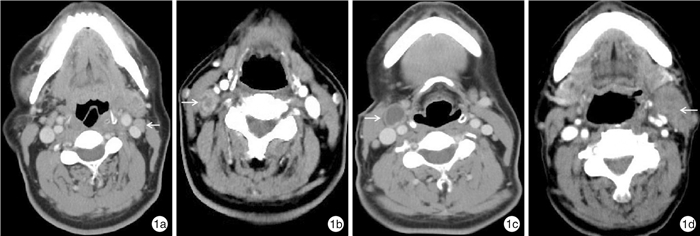
摘要: 目的 分析cN+喉鳞状细胞癌颈淋巴结转移的临床、病理特点及转移规律,探讨其诊断及处理方式。方法 从2011年3月—2021年1月于重庆医科大学附属第一医院耳鼻咽喉科手术治疗的1030例喉鳞状细胞癌患者中纳入83例cN+患者进行临床资料及随访资料的回顾性分析。结果 83例cN+喉癌中,术后pN+65例,pN-18例,cN+假阳性率为21.7%。cN+颈淋巴结转移与分型分期有关,差异有统计学意义(P < 0.05)。不同分型喉癌cN+假阳性率,声门型57.7%(16/27),声门上型3.9%(2/55)。随T分期增加,假阳性率降低。不同CT影像学特征的假阳性率:①大小:2个以上临界淋巴结为27.3%(3/11),淋巴结1~3 cm为29.4%(15/51),淋巴结>3 cm无假阳性(0/21);②强化类型:均匀强化为34.3%(12/35),不均匀强化为31.6%(6/19),环形强化为0%(0/29);③淋巴结形态及边界不清为0(0/24)。择区颈淋巴结清扫术(SND)组颈部复发率为2.4%,非SND组为20.0%,复发部位均在手术区域内。SND组和非SND组的3年颈部区域控制率分别为93.7%和81.1%,差异有统计学意义(P < 0.05)。pN+组和pN-组3年累积生存率为75.5%和87.5%,其差异无统计学意义(P>0.05)。淋巴结包膜外侵犯(ENE)组和ENE-组3年累积生存率分别为50.6%和79.3%,差异有统计学意义(P < 0.05)。结论 cN+喉癌存在假阳性,并与肿瘤分型分期有关。术前影像学对cN+的诊断不宜过度依赖大小,应结合环形强化和边界不清等淋巴结转移的特异性表现。恰当应用SND治疗cN+喉癌安全有效,并可减少过度治疗的风险。pN+喉癌患者,术后给予补充治疗能提高颈部控制率及生存率。但ENE+患者即使进行术后治疗,仍然是影响预后的不利因素。Abstract: Objective To analyze the clinical, pathological features and metastatic regularity of cervical lymph node metastasis in cN+ laryngeal squamous cell carcinoma, and to explore its diagnosis and management.Methods Among 1030 patients with laryngeal squamous cell carcinoma who underwent surgery in the Department of Otolaryngology, The First Affiliated Hospital of Chongqing Medical University from March 2011 to January 2021, 83 patients with cN+ were included in the retrospective analysis of clinical data and follow-up data.Results Among the 83 cases of cN+ laryngeal carcinoma, there were pN+65 cases and pN-18 cases. The false positive rate of cN+ was 21.7%. cN+ cervical lymph node metastasis was related to classification and staging, and the difference was statistically significant(P < 0.05).The false positive rate of cN+ in different types of laryngeal carcinoma was 57.7% (16/27) in glottic type and 3.9% (2/55) in supraglottic type. With the increase of T stage, the false positive rate decreased.The false positive rates of different CT imaging features were as follows: ①Size: the critical lymph nodes of more than 2 sizes were 27.3% (3/11), the 1~3 cm of lymph nodes was 29.4% (15/51), and the lymph nodes > 3 cm were not false positive (0/21);②The enhancement types of uniform enhancement, non-uniform enhancement and circular enhancement were 34.3% (12/35), 31.6% (6/19) and 0% (0/29) respectively. ③The proportion of unclear shape and boundary of lymph nodes was 0(0/24).The neck recurrence rate was 2.4% in the selective neck dissection (SND) and 20.0% in the non-SND. The 3-year neck area control rates of SND and non-SND group were 93.7% and 81.1% respectively, and the difference was statistically significant (P < 0.05). The 3-year cumulative survival rates of pN+ group and pN-group were 75.5% and 87.5%, respectively, and there was no significant difference between the two groups (P > 0.05). The 3-year cumulative survival rates of lymph node extranodal extension ENE+ group and ENE-group were 50.6% and 79.3%, respectively, and the difference was statistically significant (P < 0.05).Conclusion There is false positive in cN+ laryngeal carcinoma, which is related to tumor classification and staging. Preoperative imaging diagnosis of cN+ should not be over-dependent on size, but should be combined with the specific manifestations of lymph node metastasis such as circular enhancement and unclear boundaries. Proper use of SND in the treatment of cN+ laryngeal carcinoma is safe and effective, and reduces the risk of overtreatment. In patients with pN+ laryngeal carcinoma, postoperative supplementary treatment can improve the neck control rate and survival rate. However, even if postoperative treatment is performed in patients with ENE+, it is still an unfavorable factor affecting the prognosis.
-

-
表 1 cN+喉癌不同临床特征的假阳性率
特征 例数 假阳性(%) P 喉癌分型 < 0.01 声门型 27 16(57.7) 声门上型 55 2(3.9) 分化程度 >0.05 低分化 16 3(18.7) 中分化 54 10(18.5) 高分化 13 5(38.5) 声门型T分期 < 0.05 T1 0 0 T2 10 9(90.0) T3 7 4(57.1) T4a 10 3(30.0) 声门上分期 - T1 3 1(33.3) T2 7 0(0) T3 33 1(4.2) T4a 11 0(0) 淋巴结大小/cm - < 1 11 3(27.3) 1~3 51 15(29.4) >3 21 0(0) 强化类型 - 均匀强化 35 12(34.3) 不均匀强化 19 6(31.6) 环形强化 29 0(0) 形态及界限规则 59 18(47.5) - 形态及界限不规则 24 0(0) 注:T1声门型未行颈清扫,声门下型病例太少,未纳入统计指标。 表 2 pN+淋巴结分布特征
例 分型 Ⅰ Ⅱ Ⅲ Ⅳ Ⅴ Ⅵ 声门上型 1 144 59 12 1 1 声门型 0 20 10 2 0 3 声门下型 0 1 1 0 0 0 合计 1 165 70 14 1 4 表 3 cN+喉癌患者Cox比例风险分析结果
项目 B SE Wald P Exp(B) 95%CI 喉癌类型 -1.526 0.780 3.832 0.050 0.217 0.047~1.002 淋巴结转移 0.098 0.832 0.014 0.906 1.103 0.216~5.630 颈清扫类型 -0.530 0.552 0.920 0.337 0.589 0.200~1.738 包膜外侵犯 -1.029 0.489 4.438 0.035 0.357 0.137~0.931 术后治疗 0.311 0.481 0.417 0.518 1.364 0.532~3.500 -
[1] 胡晨, 张明, 薛继尧, 等. cN0声门上型喉癌的颈淋巴结隐匿性转移及处理[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(7): 615-617. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202007010.htm
[2] 沈楚霞, 李彦仕, 王志海, 等. cN0喉癌颈淋巴转移的特征分析[J]. 中华耳鼻咽喉头颈外科杂志, 2019, 54(5): 343-348. doi: 10.3760/cma.j.issn.1673-0860.2019.05.006
[3] van den Brekel MW, Stel HV, Castelijns JA, et al. Cervical lymph node metastasis: assessment of radiologic criteria[J]. Radiology, 1990, 177(2): 379-384. doi: 10.1148/radiology.177.2.2217772
[4] Khoueir N, Matar N, Farah C, et al. Survival of T4aN0 and T3N+ laryngeal cancer patients: a retrospective institutional study and systematic review[J]. Am J Otolaryngol, 2015, 36(6): 755-762. doi: 10.1016/j.amjoto.2015.07.009
[5] Coskun HH, Medina JE, Robbins KT, et al. Current philosophy in the surgical management of neck metastases for head and neck squamous cell carcinoma[J]. Head Neck, 2015, 37(6): 915-926. doi: 10.1002/hed.23689
[6] Simental AA Jr, Duvvuri U, Johnson JT, et al. Selective neck dissection in patients with upper aerodigestive tract cancer with clinically positive nodal disease[J]. Ann Otol Rhinol Laryngol, 2006, 115(11): 846-849. doi: 10.1177/000348940611501109
[7] Sumi M, Kimura Y, Sumi T, et al. Diagnostic performance of MRI relative to CT for metastatic nodes of head and neck squamous cell carcinomas[J]. J Magn Reson Imaging, 2007, 26(6): 1626-633. doi: 10.1002/jmri.21187
[8] Baik SH, Seo JW, Kim JH, et al. Prognostic Value of Cervical Nodal Necrosis Observed in Preoperative CT and MRI of Patients With Tongue Squamous Cell Carcinoma and Cervical Node Metastases: A Retrospective Study[J]. AJR Am J Roentgenol, 2019, 213(2): 437-443. doi: 10.2214/AJR.18.20405
[9] Horváth A, Prekopp P, Polony G, et al. Accuracy of the preoperative diagnostic workup in patients with head and neck cancers undergoing neck dissection in terms of nodal metastases[J]. Eur Arch Otorhinolaryngol, 2021, 278(6): 2041-2046. doi: 10.1007/s00405-020-06324-w
[10] de Bondt RB, Nelemans PJ, Hofman PA, et al. Detection of lymph node metastases in head and neck cancer: a meta-analysis comparing US, USgFNAC, CT and MR imaging[J]. Eur J Radiol, 2007, 64(2): 266-272. doi: 10.1016/j.ejrad.2007.02.037
[11] Wagner JM, Monfore N, McCullough AJ, et al. Ultrasound-Guided Fine-Needle Aspiration With Optional Core Needle Biopsy of Head and Neck Lymph Nodes and Masses: Comparison of Diagnostic Performance in Treated Squamous Cell Cancer Versus All Other Lesions[J]. J Ultrasound Med, 2019, 38(9): 2275-2284. doi: 10.1002/jum.14918
[12] Goldstein DP, Ringash J, Bissada E, et al. Scoping review of the literature on shoulder impairments and disability after neck dissection[J]. Head Neck, 2014, 36(2): 299-308. doi: 10.1002/hed.23243
[13] Andersen PE, Warren F, Spiro J, et al. Results of selective neck dissection in management of the node-positive neck[J]. Arch Otolaryngol Head Neck Surg, 2002, 128(10): 1180-1184. doi: 10.1001/archotol.128.10.1180
[14] López F, Fernández-Vañes L, García-Cabo P, et al. Selective neck dissection in the treatment of head and neck squamous cell carcinoma patients with a clinically positive neck[J]. Oral Oncol, 2020, 102: 104565. doi: 10.1016/j.oraloncology.2020.104565
[15] Rodrigo JP, Grilli G, Shah JP, et al. Selective neck dissection in surgically treated head and neck squamous cell carcinoma patients with a clinically positive neck: Systematic review[J]. Eur J Surg Oncol, 2018, 44(4): 395-403. doi: 10.1016/j.ejso.2018.01.003
[16] Tomeh C, Holsinger FC. Laryngeal cancer[J]. Curr Opin Otolaryngol Head Neck Surg, 2014, 22(2): 147-153. doi: 10.1097/MOO.0000000000000032
[17] Kolli VR, Datta RV, Orner JB, et al. The role of supraomohyoid neck dissection in patients with positive nodes[J]. Arch Otolaryngol Head Neck Surg, 2000, 126(3): 413-416. doi: 10.1001/archotol.126.3.413
[18] Patel RS, Clark JR, Gao K, et al. Effectiveness of selective neck dissection in the treatment of the clinically positive neck[J]. Head Neck, 2008, 30(9): 1231-1236. doi: 10.1002/hed.20870
[19] Barroso Ribeiro R, Ribeiro Breda E, Fernandes Monteiro E. Prognostic significance of nodal metastasis in advanced tumors of the larynx and hypopharynx[J]. Acta Otorrinolaringol Esp, 2012, 63(4): 292-298. doi: 10.1016/j.otorri.2012.02.012
-




 下载:
下载: