-
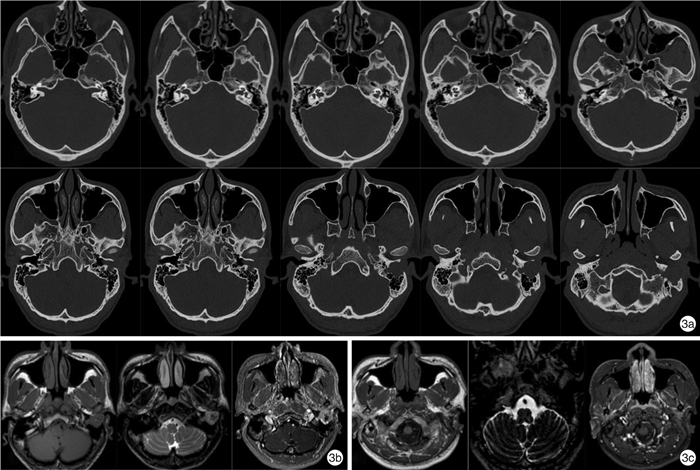
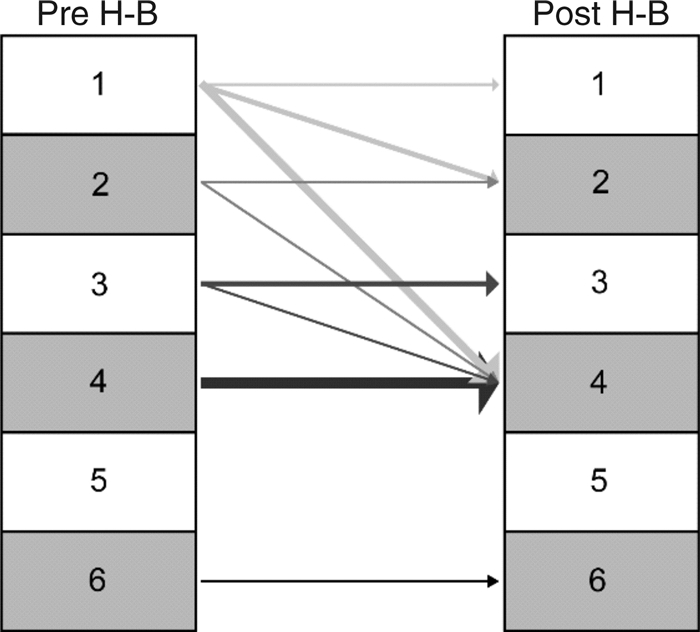
摘要: 目的 分析总结面神经鞘瘤的临床特点、手术策略选择、面神经修复方法及效果。方法 收集中山大学孙逸仙纪念医院2010年1月—2018年12月外科手术治疗的面神经鞘瘤患者的临床资料,包括面神经鞘瘤的侧别、临床表现、影像学结果、肿瘤累及范围、处理方式、术前及术后面神经功能。结果 32例面神经鞘瘤患者的主要临床表现依次为面神经麻痹(27例,84.4%)、听力下降(27例,84.4%)、耳鸣(22例,68.8%)、发现耳部肿物(15例,46.9%),耳闷塞感(13例,40.6%)等。30例患者术前诊断为面神经鞘瘤,2例患者出现术前漏诊。除1例患者随访观察外(仅行鼓室成形术),余31例均行面神经鞘瘤切除术。手术径路的选择是根据面神经鞘瘤累及的部位、范围、听功能等情况,并结合患者意愿综合考虑。31例面神经鞘瘤切除术包括经颞下窝A型入路(Fisch A)手术9例、经乳突入路手术8例、经扩大乳突入路手术7例、经乳突-颅中窝联合入路手术3例、经颅中窝入路手术1例及经颞下窝入路A型-颅中窝联合入路手术3例。28例(87.5%)患者面神经鞘瘤同时累及面神经多个节段,最常见受累的节段为面神经垂直段(26例,81.3%)。15例行面神经鞘瘤切除术的患者同期行面神经修复术,其中7例行耳大神经-面神经移植修复术,术后面神经功能改善4例;8例行面神经-舌下神经吻合修复术,术后面神经功能改善2例。同期修复术术后面神经功能最佳效果为H-BⅢ级。结论 面神经鞘瘤患者临床症状以面神经麻痹、听力下降为主;颞骨CT、颅脑MR平扫+增强扫描有助于明确诊断;手术切除面神经鞘瘤时,行神经修复术的患者术后面神经功能改善率显著高于未行神经修复的患者,应积极考虑行面神经修复;与面神经-舌下神经吻合修复相比,耳大神经-面神经移植修复可能是改善术后面神经功能的更佳选择。Abstract: Objective To elucidate the clinical characteristics, surgical strategy, facial nerve repair methods and outcomes of facial nerve schwannomas(FNS).Methods The clinical data of patients with FNS treated between January 2010 and December 2018 at Sun Yat-sen Memorial Hospital of Sun Yat-sen University were retrospectively collected, including the sidedness of FNS, clinical manifestations, imaging data, the extent of tumor, clinical management, preoperative and postoperative facial nerve function.Results The major clinical manifestations of the 32 patients with FNS were facial palsy(27, 84.4%), hearing loss(27, 84.4%), tinnitus(22, 68.8%), ear mass(15, 46.9%), and stuffy feeling in the ear(13, 40.6%) respectively. Thirty patients were preoperatively diagnosed with FNS and 2 patients were misdiagnosed. 31 patients underwent resection of FNS, except one patient who was selected for long-term follow-up observation. The choice of surgical approach was based on the location, extent and auditory function of the FNS involved as well as the patient's wishes. The surgical approach was decided based on the location and extent of the tumor: 9 patients were operated via the inferior temporal fossa type A(Fisch A) approach; 8 patients were operated via the mastoid approach; 7 patients were operated via the enlarged mastoid approach; 3 patients were operated via the combined mastoid-cranial middle fossa approach; 1 patient was operated via the cranial middle fossa approach; 3 patients were operated via the combined Fisch A-cranial middle fossa approach. 28 patients(87.5%) had FNS with multiple segments of facial nerve involved. The most involved segment was the vertical segment of the facial nerve(26, 81.3%). 15 patients underwent facial nerve repair simultaneously, including 7 cases of auricular nerve-facial nerve graft and 8 cases of facial nerve-sublingual nerve anastomosis. 4 cases had improved facial nerve function after auricular nerve-facial nerve graft and 2 cases had improved function after facial nerve-sublingual nerve anastomosis. Among patients who underwent facial nerve repair, the best outcome was H-B Ⅲ.Conclusion The patients with FNS mainly presented with facial palsy and hearing loss. Temporal bone CT and cranial MR plain & enhanced scan served well to confirm the diagnosis. The improvement rate of postoperative facial nerve function was significantly higher in patients who underwent nerve repair than in those who did not. Hence, facial nerve repair should be considered. Compared with facial nerve-sublingual nerve anastomosis, auricular major nerve-facial nerve graft might be a better choice for improving postoperative facial nerve function.
-

-
表 1 31例面神经鞘瘤患者手术治疗情况
例序 性别 年龄 患侧听力情况 手术径路 是否行神经修复 诊治年份 1 女 48 正常听力 经左颅中窝径路 未行神经修复 2017 2 男 50 正常听力 经左Fisch A-颅中窝径路 耳大、面神经移植 2016 3 女 59 重度混合性聋 经左Fisch A-颅中窝径路 耳大、面神经移植 2017 4 男 33 重度混合性聋 经右扩大乳突径路 未行神经修复 2018 5 男 40 中重度混合性聋 经左颅中窝-乳突联合径路 未行神经修复 2010 6 女 61 极重度混合性聋 经左Fisch A-颅中窝径路 面、舌下神经吻合 2013 7 男 34 轻度混合性听力下降 经左扩大乳突径路 面、舌下神经吻合 2015 8 男 60 中度混合性聋 经右扩大乳突径路 面、舌下神经吻合 2016 9 女 42 中度混合性聋 经右扩大乳突径路 未行神经修复 2010 10 女 66 极重度聋 经右扩大乳突径路 面、舌下神经吻合 2018 11 男 45 中度混合性聋 经右扩大乳突径路 耳大、面神经移植 2016 12 男 46 中度传导性聋 经右Fisch A径路 耳大、面神经移植 2010 13 男 34 中重度混合性聋 经左Fisch A径路 未行神经修复 2013 14 男 52 重度混合性聋 经右乳突径路 未行神经修复 2014 15 男 36 中度传导性聋 经左乳突径路 未行神经修复 2010 16 男 22 中重度混合性聋 经左乳突径路 未行神经修复 2014 17 女 24 正常听力 经右乳突径路 未行神经修复 2017 18 男 28 重度传导性聋 经右扩大乳突径路 面、舌下神经吻合 2010 19 女 81 极重度混合性聋 经左乳突径路 未行神经修复 2017 20 女 33 重度混合性聋 经右Fisch A径路 未行神经修复 2010 21 女 40 中度混合性聋 经左Fisch A径路 未行神经修复 2011 22 女 54 中度混合性聋 经右乳突径路 耳大、面神经移植 2010 23 女 25 中度传导性聋 经左Fisch A径路 面、舌下神经吻合 2010 24 女 31 正常听力 经左Fisch A径路 耳大、面神经移植 2016 25 女 33 重度混合性聋 经右Fisch A径路 未行神经修复 2015 26 男 22 中度混合性聋 经左Fisch A径路 耳大、面神经移植 2017 27 女 39 中度传导性聋 经右Fisch A径路 未行神经修复 2010 28 女 50 轻度传导性聋 经右乳突径路 未行神经修复 2010 29 男 29 中度传导性聋 经左乳突径路 未行神经修复 2018 30 女 42 重度混合性聋 经左颅中窝-乳突联合径路 面、舌下神经吻合 2012 31 男 20 正常听力 经右颅中窝-乳突联合径路 面、舌下神经吻合 2016 -
[1] Carlson ML, Deep NL, Patel NS, et al. Facial Nerve Schwannomas: Review of 80 Cases Over 25 Years at Mayo Clinic[J]. Mayo Clin Proc, 2016, 91(11): 1563-1576. doi: 10.1016/j.mayocp.2016.07.007
[2] House JW, Brackmann DE. Facial nerve grading system[J]. Otolaryngol Head Neck Surg, 1985, 93(2): 146-147. doi: 10.1177/019459988509300202
[3] 塞娜, 韩维举, 王萌萌, 等. 面神经鞘瘤110例临床诊断及外科治疗分析[J]. 中华耳鼻咽喉头颈外科杂志, 2019, 54(2): 101-109.
[4] Xu F, Pan S, Alonso F, et al. Intracranial Facial Nerve Schwannomas: Current Management and Review of Literature[J]. World Neurosurg, 2017, 100: 444-449. doi: 10.1016/j.wneu.2016.09.082
[5] 韩曙光, 龚树生, 王林娥. 颞骨高分辨率CT对面神经垂直段前移的判断[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(1): 17-19. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202101004.htm
[6] Rubin DI. Needle electromyography: Basic concepts[J]. Handb Clin Neurol, 2019, 160: 243-256.
[7] Shirazi MA, Leonetti JP, Marzo SJ, et al. Surgical management of facial neuromas: lessons learned[J]. Otol Neurotol, 2007, 28(7): 958-963. doi: 10.1097/MAO.0b013e3181461c8d
[8] Lahlou G, Nguyen Y, Russo FY, et al. Intratemporal facial nerve schwannoma: clinical presentation and management[J]. Eur Arch Otorhinolaryngol, 2016, 273(11): 3497-3504. doi: 10.1007/s00405-015-3850-z
[9] Quesnel AM, Santos F. Evaluation and Management of Facial Nerve Schwannoma[J]. Otolaryngol Clin North Am, 2018, 51(6): 1179-1192. doi: 10.1016/j.otc.2018.07.013
[10] Jandali D, Revenaugh PC. Facial reanimation: an update on nerve transfers in facial paralysis[J]. Curr Opin Otolaryngol Head Neck Surg, 2019, 27(4): 231-236. doi: 10.1097/MOO.0000000000000543
[11] Falcioni M, Taibah A, Russo A, et al. Facial nerve grafting[J]. Otol Neurotol, 2003, 24(3): 486-489. doi: 10.1097/00129492-200305000-00022
[12] 高伟, 卢连军, 温立婷, 等. 颞骨岩部胆脂瘤的手术治疗及面神经功能保护[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(2): 97-100. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201902001.htm
[13] Perez R, Chen JM, Nedzelski JM. Intratemporal facial nerve schwannoma: a management dilemma[J]. Otol Neurotol, 2005, 26(1): 121-126. doi: 10.1097/00129492-200501000-00022
[14] Minovi A, Vosschulte R, Hofmann E, et al. Facial nerve neuroma: surgical concept and functional results[J]. Skull Base, 2004, 14(4): 195-201. doi: 10.1055/s-2004-860948
[15] McRackan TR, Wilkinson EP, Rivas A. Primary tumors of the facial nerve[J]. Otolaryngol Clin North Am, 2015, 48(3): 491-500. doi: 10.1016/j.otc.2015.02.008
[16] Spector JG. Neural repair in facial paralysis: clinical and experimental studies[J]. Eur Arch Otorhinolaryngol, 1997, 254 Suppl 1: S68-S75.
[17] Günther M, Danckwardt-Lillieström N, Gudjonsson O, et al. Surgical treatment of patients with facial neuromas--a report of 26 consecutive operations[J]. Otol Neurotol, 2010, 31(9): 1493-1497. doi: 10.1097/MAO.0b013e3181f0c524
[18] Bartindale M, Heiferman J, Joyce C, et al. Facial Schwannoma Management Outcomes: A Systematic Review of the Literature[J]. Otolaryngol Head Neck Surg, 2020, 163(2): 293-301. doi: 10.1177/0194599820913639
[19] Liu P, Zhang Z, Liao C, et al. Dynamic Quantitative Assessment of Motor Axon Sprouting after Direct Facial-Hypoglossal End-To-Side Neurorrhaphy in Rats[J]. J Reconstr Microsurg, 2018, 34(6): 436-445. doi: 10.1055/s-0038-1636539
-

| 引用本文: | 熊颖, 梁茂金, 陈穗俊, 等. 32例面神经鞘瘤临床分析[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(12): 1085-1091. doi: 10.13201/j.issn.2096-7993.2021.12.006 |
| Citation: | XIONG Ying, LIANG Maojin, CHEN Suijun, et al. Clinical analysis of 32 cases of facial nerve schwannomas[J]. J Clin Otorhinolaryngol Head Neck Surg, 2021, 35(12): 1085-1091. doi: 10.13201/j.issn.2096-7993.2021.12.006 |
- Figure 1.
- Figure 2.
- Figure 3.



 下载:
下载: