Effect of CT localization of upper airway obstruction site after inducing sleep on the value of obstructive sleep apnea hypopnea syndrome and the effect of surgery
-
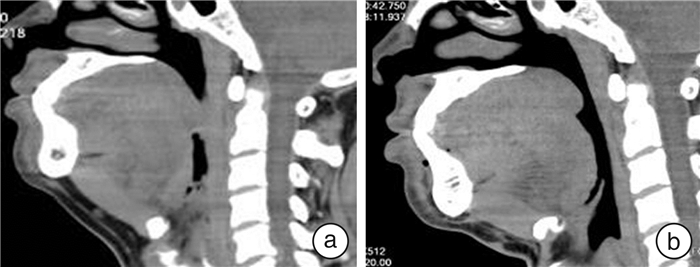
摘要: 目的 探讨诱导睡眠后上气道阻塞部位的CT定位对阻塞性睡眠呼吸暂停(OSA)患者病情及其手术疗效的评估价值。方法 对40例经多导睡眠监测确诊的中重度OSA患者先行清醒状态下上气道CT扫描;然后对患者经静脉缓慢注射右美托咪定诱导睡眠,待患者在睡眠状态下呼吸暂停时,行上气道相应部位CT扫描;比较并测量两种状态下上气道狭窄水平的截面积,评估诱导睡眠后狭窄水平截面积与患者AHI、血氧饱和度 < 90%的时间比例(CT90)的相关性。根据诱导睡眠后各解剖分区的狭窄程度将40例OSA患者分为实验1组(22例)和实验2组(18例),实验1组行低温等离子辅助改良悬雍垂腭咽成形术,实验2组行多平面联合手术;术后随访12个月,比较两组疗效、手术前后各狭窄平面截面积值的变化,以及睡眠质量相关指标的变化。结果 与清醒呼吸状态下上气道CT所测鼻咽区、软腭后区、舌根后区及会厌后区的截面积测量值比较,睡眠状态下各阻塞平面的截面积减小,差异有统计学意义(P < 0.01)。上气道各平面睡眠相最小截面积与AHI及CT90呈统计学意义负相关,其中软腭后区和舌根后区与AHI、CT90相关性较高。治疗后12个月实验1组睡眠相各区最小截面积与治疗前比较,软腭后区改善明显(P < 0.01),其次是舌根后区(P < 0.05),鼻咽区与会厌后区比较差异无统计学意义;实验2组与治疗前比较,鼻咽区、软腭后区、舌根后区、会厌后区差异均有统计学意义(P < 0.01或P < 0.05)。两组睡眠相关指标ESS、CT90、AHI、LSaO2在治疗后12个月优于治疗前,差异有统计学意义(P < 0.01)。实验1组与实验2组有效率分别为72.72%和95.23%(χ2=10.62,P < 0.01),显效率分别为58.33%和80.45%(χ2=8.62,P < 0.01),治愈率分别为12.37%和17.48%(χ2=7.62,P < 0.01)。结论 药物诱导睡眠后对OSA患者进行CT检查安全可行,其对上气道阻塞部位的准确定位具有重要价值;诱导睡眠下64排螺旋CT上气道扫描对OSA患者病情及远期手术疗效的评估具有指导意义。
-
关键词:
- 睡眠呼吸暂停,阻塞性 /
- 体层摄影术,X线计算机 /
- 诱导睡眠 /
- 悬雍垂腭咽成形术
Abstract: Objective To explore the value of CT location of the upper airway obstruction site after inducing sleep on the condition of obstructive sleep apnea(OSA) and its surgical efficacy.Methods Forty patients with moderate-to-severe OSA diagnosed by polysomnography, first performed awake CT scan, then, the patient was slowly injected intravenously with dexmedetomidine to induce sleep, when the patient was apnea during sleep, CT scan of the corresponding part of the upper airway was performed. Compare and measure the cross-sectional area of the upper airway stenosis level in the two states, and evaluate the correlation between the cross-sectional area of the stenosis level after induction of sleep and the patient's AHI, blood oxygen saturation < 90% of the time(CT90). According to the change value of the cross-sectional area of each plane, it was divided into 2 groups, 22 cases in first group underwent hypothermia plasma uvulapalatopharyngoplasty, and 18 cases in second group underwent multi-plane combined surgery. After 12 months of follow-up, compare the post-long-term efficacy, changes in cross-sectional area values of various narrow planes before and after surgery, and changes in indicators related to sleep quality between the two groups.Results Compared with the cross-sectional area of the nasopharyngeal area, posterior soft palate area, the posterior tongue area, and the epiglottis area measured by upper airway CT under awake breathing state, the cross-sectional area of each obstruction plane during sleep state decreased(P < 0.01). The minimum cross-sectional area of the upper airway plane sleep phase was negatively correlated with AHI and CT90, and the posterior soft palate and the posterior lingual base were highly correlated with AHI and CT90.12 months after treatment, the minimum cross-sectional area of each phase of the sleep phase in the experimental group 1 was significantly improved(P < 0.01) compared with that before treatment, followed by the posterior tongue area(P < 0.05). There was no statistical difference between the nasopharyngeal area and the epiglottis area. The differences in nasopharyngeal area, posterior soft palate area, posterior tongue area, and epiglottis area in experimental group 2 after treatment were statistically significant(P < 0.01 or P < 0.05), compared with that before treatment. The sleep-related indexes ESS, CT90, AHI, and LSaO2 of the two groups were better than those before treatment after 12 months of treatment(P < 0.01). Comparison of experiment group 1 and 2, the effective rates were 72.72% and 95.23%(χ2=10.62, P < 0.01), the significant efficiency was 58.33% and 80.45%(χ2=8.62, P < 0.01), and the cure rates were 12.37% and 17.48%(x2=7.62, P < 0.01).Conclusion CT examination of OSA patients after drug-induced sleep is safe and feasible, and it has important value for the accurate location of the upper airway obstruction site. 64-slice spiral CT upper airway scanning under induced sleep has guiding significance for the evaluation of OSA patients' condition and long-term surgical efficacy. -

-
表 1 实验1组和实验2组的一般资料比较
x±s 组别 例数 性别 年龄/岁 BMI AHI LSaO2/% 男 女 实验1组 22 18 4 40.2±8.9 27.9±3.4 48.4±26.8 65.7±14.8 实验2组 18 15 3 38.9±9.2 26.8±3.5 45.1±21.9 68.3±16.4 表 2 上气道各平面不同时相最小截面积比较
mm2,x±s 患者状态 鼻咽区 软腭后区 舌根后区 会厌后区 清醒相 312.40±52.54 105.61±56.24 185.48±61.13 236.76±36.32 睡眠相 251.38±48.42 82.65±32.05 120.59 ±63.39 186.73±45.12 t 9.950 8.720 8.406 6.106 P < 0.01 < 0.01 < 0.01 < 0.01 表 3 上气道各平面睡眠相最小截面积(mm2)与AHI及CT90的相关性分析
指标 鼻咽区 软腭后区 舌根后区 会厌后区 AHI r -0.477 -0.578 -0.426 -0.309 P 0.000 0.000 0.000 0.013 CT90 r -0.403 -0.524 -0.415 -0.301 P 0.001 0.000 0.000 0.019 表 4 治疗前、后上气道各平面睡眠相最小截面积比较
mm2 组别 指标 治疗前 治疗后12个月 实验1组 鼻咽区 318.22±68.43 323.66±70.21 软腭后区 65.53±26.05 152.87±52.322) 舌根后区 163.85±68.58 182.87±60.541) 会厌后区 183.22±69.67 189.13±72.20 实验2组 鼻咽区 228.39±67.43 328.28±69.812) 软腭后区 79.92±32.72 149.89±40.372) 舌根后区 119.68±69.47 191.85±75.102) 会厌后区 162.84±55.23 178.63±63.601) 与治疗前比较,1)P < 0.05,2)P < 0.01。 表 5 实验1组和实验2组治疗前后睡眠质量相关指标比较
组别 指标 治疗前 治疗后12个月 实验1组 AHI 49.4±18.8 33.8±10.91) LSaO2/% 70.3±12.3 78.8±12.31) CT90/% 18.5±10.4 11.8±6.81) ESS/分 18.5±5.8 12.9±5.21) 实验2组 AHI 48.7±21.2 23.2±9.11)2) LSaO2/% 69.9±12.1 82.8±10.31) CT90/% 19.6±9.7 9.1±5.91) ESS/分 17.8±5.2 9.1±3.61)2) 与治疗前比较,1)P < 0.01;与实验1组比较,2)P < 0.05。 -
[1] 中国医师协会睡眠医学专业委员会. 成人阻塞性睡眠呼吸暂停多学科诊疗指南[J]. 中华医学杂志, 2018, 98(24): 1902-1914. doi: 10.3760/cma.j.issn.0376-2491.2018.24.003
[2] Sutherland K, Cistulli PA. Recent advances in obstructive sleep apnea pathophysiology and treatment[J]. Sleep Biol Rhythm, 2015, 13(1): 26-40. doi: 10.1111/sbr.12098
[3] Xie C, Zhu R, Tian Y, et al. Association of obstructive sleep apnoea with the risk of vascular outcomes and all-cause mortality: a meta-analysis[J]. BMJ Open, 2017, 7(12): e013983. doi: 10.1136/bmjopen-2016-013983
[4] Huang JF, Chen GP, Wang BY, et al. Assessment of Upper-Airway Configuration in Obstructive Sleep Apnea Syndrome With Computed Tomography Imaging During Müller Maneuver[J]. Respir Care, 2016, 61(12): 1651-1658. doi: 10.4187/respcare.04669
[5] Zhang XM, Lv N, Li X, et al. The value of drug-induced sleep computed tomography in diagnosis of obstructive sleep apnea syndrome: a pilot study[J]. Acta Otolaryngol, 2019, 139(10): 895-901. doi: 10.1080/00016489.2019.1632480
[6] 周鹏, 神平, 刘稳, 等. 药物诱导睡眠内镜检查对上气道阻塞平面形态的研究[J]. 中华耳鼻咽喉头颈外科杂志, 2014, 49(1): 58-61. doi: 10.3760/cma.j.issn.1673-0860.2014.01.014
[7] Chang ET, Certal V, Song SA, et al. Dexmedetomidine versus propofol during drug-induced sleep endoscopy and sedation: a systematic review[J]. Sleep Breath, 2017, 21(3): 727-735. doi: 10.1007/s11325-017-1465-x
[8] Pahkala R, Seppä J, Ikonen A, et al. The impact of pharyngeal fat tissue on the pathogenesis of obstructive sleep apnea[J]. Sleep Breath, 2014, 18(2): 275-282. doi: 10.1007/s11325-013-0878-4
[9] 肖水芳. 舌与舌骨悬吊术[J]. 中国医学文摘(耳鼻咽喉科学), 2015, 30(3): 135-138. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYEB201503009.htm
[10] 中华医学会呼吸病学分会睡眠呼吸障碍学组. 阻塞性睡眠呼吸暂停低通气综合征诊治指南(2011年修订版)[J]. 中华结核和呼吸杂志, 2012, 35(1): 9-12. doi: 10.3760/cma.j.issn.1001-0939.2012.01.007
[11] Gagnadoux F, Jouvenot M, Meslier N, et al. [Therapeutic alternatives to continuous positive airway pressure for obstructive sleep apnea-hypopnea syndrome][J]. Presse Med, 2017, 46(4): 432-437. doi: 10.1016/j.lpm.2016.09.006
[12] Lanza A, Mariani S, Sommariva M, et al. Continuous positive airway pressure treatment with nasal pillows in obstructive sleep apnea: long-term effectiveness and adherence[J]. Sleep Med, 2018, 41: 94-99. doi: 10.1016/j.sleep.2017.08.024
[13] Tschopp S, Tschopp K. Tonsil size and outcome of uvulopalatopharyngoplasty with tonsillectomy in obstructive sleep apnea[J]. Laryngoscope, 2019, 129(12): E449-E454.
[14] Vonk PE, Rotteveel PJ, Ravesloot M, et al. The influence of position-dependency on surgical success in sleep apnea surgery-a systematic review[J]. Sleep Breath, 2020, 24(2): 433-442. doi: 10.1007/s11325-019-01935-y
[15] Elkalla RS, El Mourad MB. Respiratory and hemodynamic effects of three different sedative regimens for drug induced sleep endoscopy in sleep apnea patients. A prospective randomized study[J]. Minerva Anestesiol, 2020, 86(2): 132-140.
[16] Shepherd KL, Jensen CM, Maddison KJ, et al. Relationship between upper airway and inspiratory pump muscle force in obstructive sleep apnea[J]. Chest, 2006, 130(6): 1757-1764. doi: 10.1378/chest.130.6.1757
[17] Oliven R, Cohen G, Dotan Y, et al. Alteration in upper airway dilator muscle coactivation during sleep: comparison of patients with obstructive sleep apnea and healthy subjects[J]. J Appl Physiol(1985), 2018, 124(2): 421-429. doi: 10.1152/japplphysiol.01067.2016
[18] Bosco G, Pérez-Martín N, Morato M, et al. Nasal Surgery May Improve Upper Airway Collapse in Patients With Obstructive Sleep Apnea: A Drug-Induced Sleep Endoscopy Study[J]. J Craniofac Surg, 2020, 31(1): 68-71. doi: 10.1097/SCS.0000000000005865
[19] Socarras MA, Landau BP, Durr ML. Diagnostic techniques and surgical outcomes for persistent pediatric obstructive sleep apnea after adenotonsillectomy: A systematic review and meta-analysis[J]. Int J Pediatr Otorhinolaryngol, 2019, 121: 179-187. doi: 10.1016/j.ijporl.2019.02.030
[20] 项晋昆, 叶京英, 常青林, 等. 上气道CT软组织测量值与阻塞性睡眠呼吸暂停低通气综合征病情程度的关系[J]. 中华耳鼻咽喉头颈外科杂志, 2010, 45(5): 387-392. doi: 10.3760/cma.j.issn.1673-0860.2010.05.009
[21] Yamamoto T, Fujii N, Nishimura Y, et al. Mechanisms Underlying Improvement in Obstructive Sleep Apnea Syndrome by Uvulopalatopharyngoplasty[J]. Case Rep Otolaryngol, 2017, 2017: 2120165.
[22] Verse T, Dreher A, Heiser C, et al. ENT-specific therapy of obstructive sleep apnoea in adults: A revised version of the previously published German S2e guideline[J]. Sleep Breath, 2016, 20(4): 1301-1311. doi: 10.1007/s11325-016-1353-9
-




 下载:
下载: