-
摘要: 目的 探讨婴儿舌根囊肿合并喉软化症的诊疗策略。方法 回顾性分析36例舌根囊肿患儿的资料, 其中12例合并喉软化症。结果 所有舌根囊肿均完全切除, 术后随访半年无复发。12例合并喉软化症患儿术后入ICU插管, 1例在术后第1天时脱管, 因当时呼吸平稳、喘鸣消失未予插回, 术后第5天再次出现喉喘鸣, 术后1个月接受了修正手术, 术后插管5 d, 恢复情况好; 1例在5 d后拔管仍有较明显的喉喘鸣, 复查喉镜见声门形态尚可, 未予处置, 1个月复诊时喘鸣明显好转; 1例术后第4天脱管, 死亡。随访半年, 合并喉软化症的舌根囊肿手术有效率为83.33%。结论 舌根囊肿合并喉软化症在临床上并不少见, 两者相似的症状可能导致舌根囊肿掩盖了潜在的喉软化症, 单纯行舌根囊肿切除术可能会影响手术疗效, 有必要在手术切除舌根囊肿后进一步探查鉴别是否存在喉软化症并做出相应的处理。对于无法在术中判断是否合并Ⅲ型喉软化症的患儿, 使用低温等离子消融少量会厌谷的黏膜可能是更微创的策略。Abstract: Objective To explore the diagnosis and therapeutic strategy of laryngomalacia associated with tongue base cyst in infants.Methods A retrospective analysis was performed on 36 cases of tongue base cyst including 12 cases with concurrent laryngomalacia.Results All the cysts of the tongue base were completely resected, and no recurrence occurred during the 6-months follow-up. Twelve patients with laryngomalacia were intubated in the ICU after surgery. Tube detachment occurred in one patient in the 1st day after surgery and no reintubation was performed immediately because of stable breathing and the absence of stridor. However, the stridor occurred again in the 5th day after surgery, and revision surgery was performed 1 month after surgery. One patient still had obvious stridor after extubation in the 5th day after sugery, but the shape of glottis was good by laryngoscopy, the stridor was significantly improved at one-month follow-up. One patient died in the 4th day after the operation. The efficiency of surgical treatment in pediatric patients with tongue base cyst and concurrent laryngomalacia was 83.33%.Conclusion Laryngomalacia combined with tongue base cyst is not uncommon in clinical practice. The symptoms of tongue base cyst may mask those of the underlying laryngomalacia, since their symptoms are highly similar. Simple resection of tongue base cyst may affect the outcome of treatment. Surgeons should further investigate and identify the presence of laryngomalacia after surgical resection of the tongue base cyst and make corresponding management. For type Ⅲ laryngomalacia that cannot be determined intraoperatively, low-temperature plasma ablation of mucosa in the epiglottic valley may be a more minimally invasive option.
-
Key words:
- tongue base cyst /
- laryngomalacia /
- infant
-

-
表 1 12例舌根囊肿合并喉软化症患儿的资料
例序 性别 年龄 主诉 合并症 术前纤维喉镜检查 术中支撑喉镜下切除舌根囊肿后 声门上成形术类型 术后情况 术后1个月 1 女 10个月21天 喉喘鸣10个月 睡眠打鼾 舌根囊肿,杓会厌皱襞短缩 杓会厌皱襞短缩 Ⅱ 插管入ICU,5 d后拔管喉喘鸣消失 复查情况好 2 男 1个月24天 喉喘鸣1个月 呼吸困难,Ⅰ度喉梗阻 舌根囊肿,杓会厌皱襞短缩 杓会厌皱襞短缩 Ⅱ 插管入ICU,因肺炎延长至8 d拔管,拔管后喉喘鸣消失,喉梗阻消失 复查情况好 3 男 1个月26天 出生后喉喘鸣 呛奶,房间隔缺损,卵圆孔未闭 舌根囊肿,杓会厌皱襞短缩 杓会厌皱襞短缩 Ⅱ 插管入ICU,5 d拔管后喉喘鸣消失,仍有呛奶 复查情况好,呛奶好转 4 男 1个月29天 喉喘鸣1个月 呼吸困难,Ⅱ度喉梗阻 舌根囊肿,披裂黏膜脱垂、杓会厌皱襞短缩 披裂黏膜脱垂、杓会厌皱襞短缩 Ⅰ+Ⅱ 插管入ICU,5 d后拔管喉喘鸣和喉梗阻明显好转 复查情况好,喉喘鸣和喉梗阻消失 5 男 5个月27天 喉喘鸣5个月 无 舌根囊肿,披裂黏膜脱垂 披裂黏膜脱垂 Ⅰ 插管入ICU,5 d后拔管喉喘鸣明显好转 复查情况好,喉喘鸣消失 6 女 3个月6天 出生后喉喘鸣 无 舌根囊肿,会厌倒伏,声门暴露欠佳 无明显异常 Ⅲ 术后拔管,喉喘鸣仍明显,喉镜下见会厌倒伏,转入ICU插管,因肺炎延长至8 d拔管,拔管后喉喘鸣消失 复查情况好,喉喘鸣消失 7 女 4个月 出生后喉喘鸣 呼吸困难 舌根囊肿,会厌倒伏,声门暴露欠佳 无明显异常 Ⅲ 术后拔管,术后第1天再次出现喉喘鸣,喉镜下见会厌倒伏,转入ICU插管,第4天脱管,死亡 - 8 男 2个月10天 出生后喉喘鸣 呼吸困难,Ⅱ度喉梗阻,神经发育不全,房间隔缺损 舌根囊肿,会厌倒伏,声门暴露欠佳 无明显异常 Ⅲ 术后拔管,喉喘鸣仍明显,喉镜下见会厌倒伏,转入ICU插管,5 d后拔管喉喘鸣好转,喉梗阻明显好转 复查情况好,喉喘鸣明显好转,喉梗阻消失 9 男 1个月22天 喉喘鸣1个月 无 舌根囊肿,会厌倒伏,声门暴露欠佳 无明显异常 Ⅲ 术后拔管,喉喘鸣仍明显,喉镜下见会厌倒伏,转入ICU插管,5 d后拔管仍有喉喘鸣,喉镜下见声门形态尚可 复查情况好,喉喘鸣明显好转 10 男 3个月14天 出生后喉喘鸣 无 舌根囊肿,会厌倒伏,声门暴露欠佳 杓会厌皱襞短缩 Ⅱ+Ⅲ 插管入ICU,因肺炎延长至8 d拔管,拔管后喉喘鸣消失 复查情况好,喉喘鸣消失 11 女 1个月12天 出生后喉喘鸣 呼吸困难,Ⅱ度喉梗阻 舌根囊肿,会厌倒伏,声门暴露欠佳 杓会厌皱襞短缩 Ⅱ+Ⅲ 插管入ICU,5 d后拔管喉喘鸣明显好转 复查情况好,喉喘鸣消失 12 男 4个月5天 喉喘鸣3月余 无 舌根囊肿,会厌倒伏,声门暴露欠佳 披裂黏膜肥厚、杓会厌皱襞短缩 Ⅰ+Ⅱ+Ⅲ 插管入ICU,术后第1天脱管,患儿呼吸平稳,无喘鸣,未插回,术后第5天喘鸣加重 复查仍有明显喉喘鸣,喉镜下见会厌倒伏,杓会厌皱襞短缩,予修正手术,再次插管,5 d后拔管效果好 -
[1] Daniel SJ. The upper airway: congenital malformations[J]. Paediatr Respir Rev, 2006, 7 Suppl 1: S260-263.
[2] Bedwell J, Zalzal G. Laryngomalacia[J]. Semin Pediatr Surg, 2016, 25(3): 119-122. doi: 10.1053/j.sempedsurg.2016.02.004
[3] Thompson DM. Abnormal sensorimotor integrative function of the larynx in congenital laryngomalacia: a new theory of etiology[J]. Laryngoscope, 2007, 117(6 Pt 2 Suppl 114): 1-33.
[4] Bedwell J, Zalzal G. Laryngomalacia[J]. Semin Pediatr Surg, 2016, 25(3): 119-122. doi: 10.1053/j.sempedsurg.2016.02.004
[5] Wright CT, Goudy SL. Congenital laryngomalacia: symptom duration and need for surgical intervention[J]. Ann Otol Rhinol Laryngol, 2012, 121(1): 57-60. doi: 10.1177/000348941212100110
[6] Olney DR, Greinwald JH Jr, Smith RJ, et al. Laryngomalacia and its treatment[J]. Laryngoscope, 1999, 109(11): 1770-1775. doi: 10.1097/00005537-199911000-00009
[7] 浦诗磊, 李晓艳, 改良声门上成形术治疗喉软化症的疗效评价[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(11): 1072-1075, 1080. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201911017.htm
[8] LimaTM, Gonçalves DU, Gonçalves LV, et al. Flexible nasolaryngoscopy accuracy in laryngomalacia diagnosis[J]. Braz J Otorhinolaryngol, 2008, 74(1): 29-32. doi: 10.1016/S1808-8694(15)30747-3
[9] 中国妇幼保健学会微创分会儿童耳鼻咽喉学组. 儿童喉软化症诊断与治疗临床实践指南[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(11): 961-965. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH202011001.htm
[10] Topf P, Fried MP, Stromen M. Vagaries of thyroglossal duct cysts[J]. Laryngoscope, 1988, 98(7): 740-742.
[11] Turri-Zanoni M, Battaglia P, Castelnuovo P. Thyroglossal Duct Cyst at the Base of Tongue: The Emerging Role of Transoral Endoscopic-Assisted Surgery[J]. J Craniofac Surg, 2018, 29(2): 469-470. doi: 10.1097/SCS.0000000000004009
[12] Carter J, Rahbar R, Brigger M, et al. International Pediatric ORL Group(IPOG)laryngomalacia consensus recommendations[J]. Int J Pediatr Otorhinolaryngol, 2016, 86: 256-261. doi: 10.1016/j.ijporl.2016.04.007
[13] Pu SL, Xu HM, Li XY. Supraglottoplasty in neonates and infants: A radiofrequency ablation approach[J]. Medicine(Baltimore), 2018, 97(7): e9850.
-

| 引用本文: | 浦诗磊, 李为, 李晓艳. 婴儿舌根囊肿合并喉软化症的诊疗策略[J]. 临床耳鼻咽喉头颈外科杂志, 2021, 35(6): 517-520. doi: 10.13201/j.issn.2096-7993.2021.06.007 |
| Citation: | PU Shilei, LI Wei, LI Xiaoyan. The management of infantile tongue base cyst with laryngomalacia[J]. J Clin Otorhinolaryngol Head Neck Surg, 2021, 35(6): 517-520. doi: 10.13201/j.issn.2096-7993.2021.06.007 |
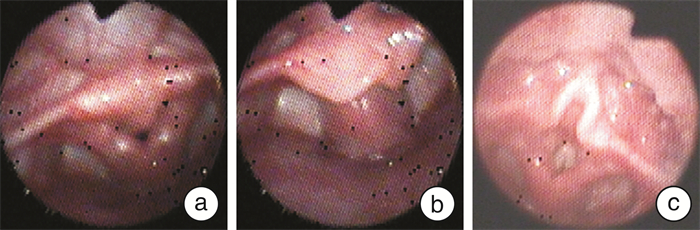
- Figure 1.



 下载:
下载: