Clinical analysis of the vascular pulsatile tinnitus associated with sigmoid sinus-mastoid
-
摘要: 目的 探讨乙状窦-乳突相关的血管性搏动性耳鸣(PT)临床诊疗特点。方法 回顾性分析自2013-2020年间由同一医生收治的45例PT患者的临床资料, 观察运用手术治疗和非手术治疗的疗效。术式: 经乳突入路乙状窦前壁骨壁重建术, 以及乳突导血管结扎术; 非手术治疗方法有抗贫血治疗和观察。门诊随访。结果 全部患者中, 女43例, 男2例; 2例女性为客观性耳鸣, 其余均为主观性耳鸣; 平均年龄42.7岁。共有40例选择手术, 其中38例选择经乳突入路乙状窦前壁骨壁重建术, 内有6例同期行乳突导血管结扎术; 其他2例行单纯乳突导血管结扎术。5例选择了非手术治疗, 其中2例抗贫血治疗, 3例观察。最长随访7年半, 最短6个月。1例失访。总治愈率80.0%(36/45), 手术治愈率82.5%(33/40), 非手术治愈率60.0%(3/5)。结论 该PT致病机制复杂且至今尚不清楚, 下述几点可能在病因中发挥重要作用: 女性、共同的解剖异常影像特征及血流动力学变化。确定PT的责任部位或主要致病因素是一个关键点。尽管术式相对简单, 效果显著且并发症轻微, 但是手术可能并不是唯一的治疗选择。Abstract: Objective To probe the clinical characteristics of diagnosis and therapy of vascular pulsatile tinnitus(PT) associated with sigmoid sinus-mastoid.Methods Retrospectively analyzed the clinical data of the hospitalized 45 PT patients of an ear surgeon in one hospital between January 2013 to January 2020, and observed the effectiveness with surgery and non-surgery therapy. Surgical procedures include reconstruction the bone wall of sigmoid sinus by transmastoid approach and ligation of mastoid emissary vein. Non-surgery therapy includes anti-anemia therapy and observation. All patients have been followed-up in ENT outpatient.Results Of 45 cases, female : male was 43: 2, the mean age was 42.7 years old. The other PT patients were the subjective tinnitus except two females were the objective tinnitus. Of 40 cases, 38 patients underwent transmastoid approach to reconstructed sigmoid sinus bone wall, including 6 patients with the ligated mastoid emissary vein at the same period.The other 2 cases with the ligated mastoid emissary vein only.Five cases were treated by non-surgery therapies, including 2 cases anti-anemia therapy and 3 cases observation. The longest follow-up period was seven and a half years, the shortest was six months. One case was lost to follow up. The total cure rate was 80.0%(36/45), the surgery cure rate was 82.5%(33/40), the non-surgery cure rate was 60.0% (3/5).Conclusion The pathophysiologic mechanism of the PT is still complex and unclear until now. However, the following conditions probably play an important role in the etiology: female, common features of anatomy anomalies, hemodynamic variations. It is a key point to confirm the responsible site or the main cause of the PT. Although the surgery is relatively simple, the effect is remarkable and no major postoperative complications, surgery could not be a only choice.
-
Key words:
- pulsatile tinnitus /
- diagnosis /
- therapy
-

-
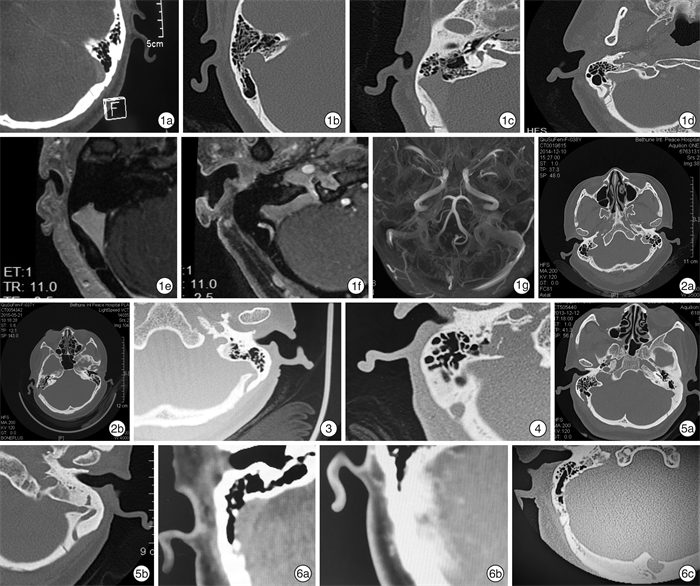
图 1 采用骨算法HRCT和头颅磁共振增强三维扰相梯度回波序列检查并做多平面重组,曲面重组等图像分析 1a:左侧乙状窦前壁骨壁缺失型;1b:右侧乙状窦憩室;1c:CT示右侧乳突导血管畸形合并乙状窦骨壁缺失;1d:CT示右侧乳突导血管畸形合并乙状窦憩室;1e:MRI示右侧乳突导血管畸形合并乙状窦骨壁缺失;1f:MRI示右侧乳突导血管畸形合并乙状窦憩室;1g:左侧乙状窦优势引流;图 2 右侧SSDD手术前(2a)和手术后(2b); 图 3 左侧乳突导血管扩大畸形内口径为4.4 mm,外口径为3.5 mm; 图 4 右侧乳突导血管畸形合并颈静脉球乳突侧憩室; 图 5 双侧乳突导血管扩大畸形 仅右侧PT(5a),左侧硬化型(5b),无PT; 图 6 右侧乙状窦前壁骨壁缺失(6a)+弥漫性动静脉瘘(6b)+蛛网膜颗粒(6c)
-
[1] Chari DA, Limb CJ. Tinnitus[J]. Med Clin North Am, 2018, 102(6): 1081-1093. doi: 10.1016/j.mcna.2018.06.014
[2] Chandler JR. Diagnosis and cure of venous hum tinnitus[J]. Laryngoscope, 1983, 93(7): 892-895.
[3] Marsot-Dupuch K. Pulsatile and nonpulsatile tinnitus: a systemic approach[J]. Semin Ultrasound CT MR, 2001, 22(3): 250-70. doi: 10.1016/S0887-2171(01)90010-1
[4] Wang AC, Nelson AN, Pino C, et al. Management of Sigmoid Sinus Associated Pulsatile Tinnitus: A Systematic Review of the Literature[J]. Otol Neurotol, 2017, 38(10): 1390-1396. doi: 10.1097/MAO.0000000000001612
[5] 杨军, 汪吉宝. 搏动性耳鸣[J]. 临床耳鼻咽喉科杂志, 1999, 13(4): 184-186. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH199904028.htm
[6] 侯志强, 韩东一. 静脉源性搏动性耳鸣[J]. 听力学及言语疾病杂志, 2011, 19(6): 573-575. https://www.cnki.com.cn/Article/CJFDTOTAL-TLXJ201106031.htm
[7] Sismanis A. Pulsatile tinnitus: contemporary assessment and management[J]. Curr Opin Otolaryngol Head Neck Surg, 2011, 19(5): 348-357. doi: 10.1097/MOO.0b013e3283493fd8
[8] 刘辛迪. 血管性搏动性耳鸣研究进展[J]. 临床耳鼻咽喉头颈外科杂志, 2017, 31(18): 1450-1454. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201718022.htm
[9] Otto KJ, Hudgins PA, Abdelkafy W, et al. Sigmoid sinus diverticulum: a new surgical approach to the correction of pulsatile tinnitus[J]. Otol Neurotol, 2007, 28(1): 48-53. doi: 10.1097/01.mao.0000247814.85829.f6
[10] Xue J, Li T, Sun X, et al. Focal defect of mastoid bone shell in the region of the transverse-sigmoid junction: a new cause of pulsatile tinnitus[J]. J Laryngol Otol, 2012, 126(4): 409-413. doi: 10.1017/S0022215111003458
[11] Grewal AK, Kim HY, Comstock RH 3rd, et al. Clinical presentation and imaging findings in patients with pulsatile tinnitus and sigmoid sinus diverticulum/dehiscence[J]. Otol Neurotol, 2014, 35(1): 16-21. doi: 10.1097/MAO.0b013e31829ab6d7
[12] Kizildag B, Bilal N, Yurttutan N, et al. The relationship between tinnitus and vascular anomalies on temporal bone CT scan: a retrospective case control study[J]. Surg Radiol Anat, 2016, 38(7): 835-841. doi: 10.1007/s00276-016-1629-6
[13] Jianu DC, Jianu SN, Dan TF, et al. Pulsatile tinnitus caused by a dilated left petrosquamosal sinus[J]. Rom J Morphol Embryol, 2016, 57(1): 319-322.
[14] Reardon MA, Raghavan P. Venous Abnormalities Leading to Tinnitus: Imaging Evaluation[J]. Neuroimaging Clin N Am, 2016, 26(2): 237-245. doi: 10.1016/j.nic.2015.12.006
[15] Lee SH, Kim SS, Sung KY, et al. Pulsatile tinnitus caused by a dilated mastoid emissary vein[J]. J Korean Med Sci, 2013, 28(4): 628-630. doi: 10.3346/jkms.2013.28.4.628
[16] Eisenman DJ, Raghavan P, Hertzano R, et al. Evaluation and treatment of pulsatile tinnitus associated with sigmoid sinus wall anomalies[J]. Laryngoscope, 2018, 128 Suppl 2: S1-S13.
[17] 曾嵘, 王国鹏, 龚树生. 搏动性耳鸣研究进展[J]. 中华耳鼻咽喉头颈外科杂志, 2011, 46(11): 957-961. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201718022.htm
[18] 刘兆会, 王振常, 张涵娟, 等. 搏动性耳鸣影像学分析思路及诊断原则的教学培训[J]. 中国耳鼻咽喉头颈外科, 2015, 22(11): 597-598. https://www.cnki.com.cn/Article/CJFDTOTAL-EBYT201511021.htm
[19] 龚树生, 曾嵘, 王国鹏. 重视乙状窦相关病变致搏动性耳鸣的诊治[J]. 临床耳鼻咽喉头颈外科杂志, 2015, 29(8): 677-680. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201508001.htm
[20] 苏天昊, 金龙, 韩燕京, 等. 搏动性耳鸣相关横窦、乙状窦狭窄及压力梯度的血管造影研究[J]. 影像诊断与介入放射学, 2019, 28(2): 118-121. https://www.cnki.com.cn/Article/CJFDTOTAL-YXZD201902011.htm
[21] 崔永华, 褚汉启, 王志斌等. 超选择动脉栓塞治疗血管搏动性耳鸣[J]. 临床耳鼻咽喉科杂志, 1998, 12(2): 61-63. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH199802005.htm
[22] 彭佳丽, 赵蓉, 李格飞, 等. 乙状窦憩室致搏动性耳鸣的介入治疗成功案例报道[J]. 上海交通大学学报(医学版), 2016, 36(12): 1820-1822. https://www.cnki.com.cn/Article/CJFDTOTAL-SHEY201612040.htm
[23] 曹向宇, 张荣举, 王君, 等. 源于乙状窦憩室搏动性耳鸣的血管内治疗[J]. 中华老年心脑血管病杂志, 2017, 19(2): 134-136. https://www.cnki.com.cn/Article/CJFDTOTAL-LNXG201702006.htm
[24] Trivelato FP, Araújo JF, Dos Santos Silva R, et al. Endovascular treatment of pulsatile tinnitus associated with transverse sigmoid sinus aneurysms and jugular bulb anomalies[J]. Interv Neuroradiol, 2015, 21(4): 548-551. doi: 10.1177/1591019915590367
[25] 孙兴旺, 崔豹, 徐卫峰, 等. 搏动性耳鸣乙状窦骨壁缺损与病程相关性研究[J]. 医学影像学杂志, 2017, 27(6): 1032-1035. https://www.cnki.com.cn/Article/CJFDTOTAL-XYXZ201706010.htm
[26] 杜昱平, 张永顺, 周永清等. 搏动性耳鸣的CT与MRI影像分析[J]. 实用放射学杂志, 2015, 31(1): 24-27. doi: 10.3969/j.issn.1002-1671.2015.01.007
[27] Hampl M, Kachlik D, Kikalova K, et al. Mastoid foramen, mastoid emissary vein and clinical implications in neurosurgery[J]. Acta Neurochir(Wien), 2018, 160(7): 1473-1482. doi: 10.1007/s00701-018-3564-2
[28] Forte V, Turner A, Liu P. Objective tinnitus associated with abnormal mastoid emissary vein[J]. J Otolaryngol, 1989, 18(5): 232-235.
[29] 刘阳云, 刘军, 姜怀洲, 等. 乳突导静脉扩大致搏动性耳鸣1例并文献复习[J]. 中华耳科学杂志, 2010, 8(2): 234-235. doi: 10.3969/j.issn.1672-2922.2010.02.026
[30] Zhao P, Lv H, Dong C, et al. CT evaluation of sigmoid plate dehiscence causing pulsatile tinnitus[J]. Eur Radiol, 2016, 26(1): 9-14. doi: 10.1007/s00330-015-3827-8
[31] Wang GP, Zeng R, Liu ZH, et al. Clinical characteristics of pulsatile tinnitus caused by sigmoid sinus diverticulum and wall dehiscence: a study of 54 patients[J]. Acta Otolaryngol, 2014, 134(1): 7-13. doi: 10.3109/00016489.2013.831479
[32] Yeo WX, Xu SH, Tan TY, et al. Surgical management of pulsatile tinnitus secondary to jugular bulb or sigmoid sinus diverticulum with review of literature[J]. Am J Otolaryngol, 2018, 39(2): 247-252. doi: 10.1016/j.amjoto.2017.12.019
[33] Santa Maria PL. Sigmoid sinus dehiscence resurfacing as treatment for pulsatile tinnitus[J]. J Laryngol Otol, 2013, 127 Suppl 2: S57-59.
[34] Sismanis A, Butts FM, Hughes GB. Objective tinnitus in benign intracranial hypertension: an update[J]. Laryngoscope, 1990, 100(1): 33-36.
[35] Lansley JA, Tucker W, Eriksen MR, et al. Sigmoid Sinus Diverticulum, Dehiscence, and Venous Sinus Stenosis: Potential Causes of Pulsatile Tinnitus in Patients with Idiopathic Intracranial Hypertension?[J]. AJNR Am J Neuroradiol, 2017, 38(9): 1783-1788. doi: 10.3174/ajnr.A5277
[36] Eisenman DJ. Sinus wall reconstruction for sigmoid sinus diverticulum and dehiscence: a standardized surgical procedure for a range of radiographic findings[J]. Otol Neurotol, 2011, 32(7): 1116-1119. doi: 10.1097/MAO.0b013e31822a1c7d
[37] 李国霖, 范圣瑾, 曲松滨. 贫血患者经颅多普勒超声的改变[J]. 中华超声影像学杂志, 2004, 13(12): 953-954. doi: 10.3760/j.issn:1004-4477.2004.12.022
[38] Weinreich HM, Carey JP. Prevalence of Pulsatile Tinnitus Among Patients With Migraine[J]. Otol Neurotol, 2016, 37(3): 244-247. doi: 10.1097/MAO.0000000000000968
-




 下载:
下载: