Postoperative prognostic risk factors and treatment strategies for patients with T3-T4 hypopharyngeal squamous cell carcinoma
-
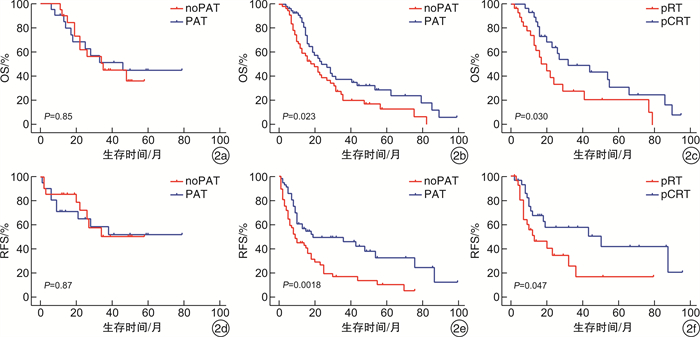
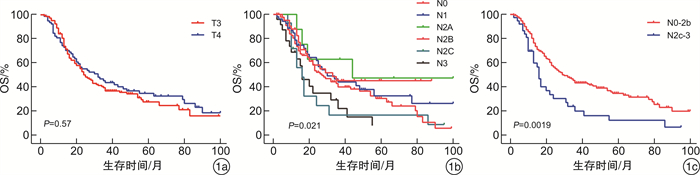
摘要: 目的 探讨T3~T4期下咽癌患者手术后预后相关风险因素以及不同术后辅助治疗策略对患者预后的影响。方法 回顾性分析2003-2015年间229例在复旦大学附属眼耳鼻喉科医院接受手术的T3~T4期下咽癌患者的临床资料。通过单、多因素分析患者术后生存的风险因素并将患者根据风险分层, 比较不同术后辅助治疗方案在不同风险组中的疗效。结果 229例T3~T4期患者3年及5年总生存率分别为39.07%、29.03%;3年及5年RFS分别为40.22%、30.29%。多因素分析结果显示咽后壁及环后区肿瘤、N2c~N3、淋巴血管侵犯以及淋巴结囊外扩散是患者预后的独立危险因素。术后辅助治疗的应用显著改善高风险组患者术后生存(P < 0.05), 并能降低术后复发(P < 0.01), 且术后放化疗效果优于单纯术后放疗(P < 0.05)。术后辅助治疗对低风险组患者术后生存没有显著影响。结论 T3~T4期下咽癌患者预后的独立风险因素包括咽后壁及环后区肿瘤、N2c~N3、淋巴血管侵犯以及淋巴结囊外扩散。建议存在风险因素的患者接受术后辅助治疗, 其中术后放化疗优于单纯术后放疗。对于无风险因素的患者, 术后建议密切随访及复查。Abstract: Objective To investigate the independent prognostic risk factors and the application of different postoperative adjuvant treatment strategies on patients with T3-T4 hypopharyngeal carcinoma.Methods Based on the inclusion criteria, we conducted a retrospective study that analyzed the clinical data of 229 cases who underwent surgery at the Eye, Ear, Nose and Throat Hospital of Fudan University from 2003 to 2015. Risk factors for postoperative survival were analyzed by univariate and multivariate analysis and patients were stratified according to the independent risk factors. The efficacy of various postoperative adjuvant therapystrategies were compared in different risk groups.Results Two hundred and twenty-nine patients with T3-T4 primary tumor had 3-year and 5-year overall survival rates of 39.07% and 29.03%, respectively; 3-year and 5-year recurrence-free survival rates were 40.22% and 30.29%, respectively. The results of multivariate analysis demonstrated that tumors in the posterior pharyngeal wall and posterior cricoid region, N2c-N3, lymphovascular invasion, and extranodal extension were independent risk factors. The utility of postoperative adjuvant therapy significantly improved postoperative survival in the high-risk group (P < 0.05) and reduced postoperative recurrence significantly (P < 0.01). Patients received adjuvant chemoradiation had better survival than those received adjuvant radiation alone (P < 0.05). Postoperative adjuvant therapy had no significant effect on postoperative survival of patients in the low-risk group.Conclusion Independent risk factors for patients with T3-T4 hypopharyngeal carcinoma include tumors in the posterior pharyngeal wall and posterior cricoid region, N2c-N3, lymphovascular invasion, as well as extranodal extension. Postoperative adjuvant therapy, especially adjuvant chemoradiation, is recommended for patient with risk factors mentioned above. For patients without those risk factors, postoperative follow-up and re-examination are recommended.
-

-
表 1 T3~T4期下咽癌患者临床病理特征
病理特征 例数(%) 病理特征 例数(%) 年龄/岁 N分期 <60 122(53.28) N0 42(18.34) ≥60 107(46.72) N1 53(23.14) 性别 N2 110(48.03) 女性 5(2.18) N3 24(10.48) 男性 224(97.82) 肿瘤分化程度 吸烟史 高/中分化 212(92.58) 无 78(34.06) 低分化 17(7.42) 有 151(65.94) 淋巴血管侵犯 饮酒史 无 197(86.03) 无 107(46.72) 有 32(13.97) 有 122(53.28) 淋巴结囊外扩散 解剖亚区 无 130(56.77) 梨状窝区 183(79.91) 有 99(43.23) 环后区 17(7.42) 切缘状态 咽后壁区 29(12.66) 阳性 25(10.92) T分期 阴性 204(89.08) T3 148(64.63) 术后辅助治疗 T4 81(35.37) 无 96(41.92) 术后放疗 57(24.89) 术后放化疗 76(33.19) 表 2 T3~T4期下咽癌患者预后的单多因素分析
项目 单因素分析 多因素分析 HR(95%CI) P HR(95%CI) P 年龄≥60岁 0.867(0.623~1.208) 0.399 男性 2.881(0.712~11.66) 0.138 2.790(0.677~11.51) 0.156 有吸烟史 0.881(0.623~1.245) 0.471 有饮酒史 1.131(0.809~1.583) 0.471 咽后壁及环后区 1.583(1.048~2.391) 0.029 1.895(1.229~2.921) 0.004 T4期 0.902(0.638~1.275) 0.559 N2c~3期 1.903(1.262~2.868) 0.002 1.669(1.081~2.578) 0.021 肿瘤低分化 0.843(0.455~1.561) 0.586 有淋巴血管侵犯 1.945(1.256~3.013) 0.003 1.807(1.152~2.835) 0.009 有淋巴结囊外扩散 1.683(1.208~2.3440 0.002 1.612(1.128~2.303) 0.009 切缘阴性 0.653(0.387~1.101) 0.110 术后有辅助治疗 0.778(0.558~1.085) 0.139 0.711(0.502~1.005) 0.053 -
[1] Newman JR, Connolly TM, Illing EA, et al. Survival trends in hypopharyngeal cancer: a population-based review[J]. Laryngoscope, 2015, 125(3): 624-629. doi: 10.1002/lary.24915
[2] Hall SF, Groome PA, Irish J, et al. The natural history of patients with squamous cell carcinoma of the hypopharynx[J]. Laryngoscope, 2008, 118(8): 1362-1371. doi: 10.1097/MLG.0b013e318173dc4a
[3] Amin MB, Edge S, Greene F, et al. AJCC Cancer Staging Manual[M]. 8th ed. New York: Springer, 2017: 129-130.
[4] Garneau JC, Bakst RL, Miles BA. Hypopharyngeal cancer: A state of the art review[J]. Oral Oncol, 2018, 86: 244-250. doi: 10.1016/j.oraloncology.2018.09.025
[5] Habib A. Management of advanced hypopharyngeal carcinoma: systematic review of survival following surgical and non-surgical treatments[J]. J Laryngol Otol, 2018, 132(5): 385-400. doi: 10.1017/S0022215118000555
[6] 路铁, 李振东, 李树春, 等. 321例下咽癌患者临床特征及两种治疗方式疗效分析[J]. 临床耳鼻咽喉头颈外科杂志, 2019, 33(3): 275-279. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201903022.htm
[7] 耿志洋, 郑宏良. 局部晚期下咽癌的治疗进展[J]. 临床耳鼻咽喉头颈外科杂志, 2017, 31(9): 732-736. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201709025.htm
[8] 陶磊, 周梁, 张明, 等. 下咽癌预后改变及原因分析: 单中心2003—2007年与2010—2014年两个五年间数据对比[J]. 中华耳鼻咽喉头颈外科杂志, 2020, 55(2): 116-124. doi: 10.3760/cma.j.issn.1673-0860.2020.02.007
[9] Xing Y, Zhang J, Lin H, et al. Relation between the level of lymph node metastasis and survival in locally advanced head and neck squamous cell carcinoma[J]. Cancer, 2016, 122(4): 534-545. doi: 10.1002/cncr.29780
[10] Cassidy RJ, Switchenko JM, Jegadeesh N, et al. Association of Lymphovascular Space Invasion With Locoregional Failure and Survival in Patients With Node-Negative Oral Tongue Cancers[J]. JAMA Otolaryngol Head Neck Surg, 2017, 143(4): 382-388. doi: 10.1001/jamaoto.2016.3795
[11] Michikawa C, Uzawa N, Kayamori K, et al. Clinical significance of lymphatic and blood vessel invasion in oral tongue squamous cell carcinomas[J]. Oral Oncol, 2012, 48(4): 320-324. doi: 10.1016/j.oraloncology.2011.11.014
[12] 邸斌, 李晓明, 尚耀东, 等. 影响下咽癌患者复发及其预后的临床病理学因素[J]. 中华耳鼻咽喉头颈外科杂志, 2009, 44(9): 716-721. doi: 10.3760/cma.j.issn.1673-0860.2009.09.004
[13] Wreesmann VB, Katabi N, Palmer FL, et al. Influence of extracapsular nodal spread extent on prognosis of oral squamous cell carcinoma[J]. Head Neck, 2016, 38 Suppl 1: E1192-1199.
[14] Kim SY, Rho YS, Choi EC, et al. Clinicopathological factors influencing the outcomes of surgical treatment in patients with T4a hypopharyngeal cancer[J]. BMC Cancer, 2017, 17(1): 904. doi: 10.1186/s12885-017-3880-6
[15] Jang JY, Choi N, Ko YH, et al. Differential Impact of Close Surgical Margin on Local Recurrence According to Primary Tumor Size in Oral Squamous Cell Carcinoma[J]. Ann Surg Oncol, 2017, 24(6): 1698-1706. doi: 10.1245/s10434-016-5497-4
[16] Hinerman RW, Morris CG, Amdur RJ, et al. Surgery and postoperative radiotherapy for squamous cell carcinoma of the larynx and pharynx[J]. Am J Clin Oncol, 2006, 29(6): 613-621. doi: 10.1097/01.coc.0000242319.09994.78
[17] Langendijk JA, Ferlito A, Takes RP, et al. Postoperative strategies after primary surgery for squamous cell carcinoma of the head and neck[J]. Oral Oncol, 2010, 46(8): 577-585. doi: 10.1016/j.oraloncology.2010.03.023
[18] Heng Y, Zhu X, Zhou L, et al. The presence of risk factors and corresponding treatment strategies post-surgical resection in stage Ⅳ hypopharyngeal squamous cell carcinoma patients: a retrospective cohort study[J]. Ann Transl Med, 2020, 8(5): 189. doi: 10.21037/atm.2020.01.102
[19] 董频, 英信江, 陈歆维, 等. 新辅助化疗方案尼妥珠单抗联合奈达铂和5-氟尿嘧啶治疗下咽鳞癌初步临床分析[J]. 山东大学耳鼻喉眼学报, 2016, 30(3): 10-14. https://www.cnki.com.cn/Article/CJFDTOTAL-SDYU201603003.htm
[20] Ferris RL. Immunology and Immunotherapy of Head and Neck Cancer[J]. J Clin Oncol, 2015, 33(29): 3293-3304.
-




 下载:
下载: