-
摘要: 目的 观察不同临床表型慢性鼻窦炎(CRS)的微生物学构成特点及临床相关性研究。方法 收集行鼻内镜手术的CRS患者196例,其中慢性鼻窦炎伴鼻息肉(CRSwNP)患者126例、慢性鼻窦炎不伴鼻息肉(CRSsNP)患者70例,78例鼻中隔偏曲患者(对照组)入组。术前采集中鼻道区域鼻腔分泌物标本,利用传统培养方法进行细菌的分离及鉴定。通过Pearson卡方检验或Fisher精确检验进行两组间细菌的比较,使用Kruskal-Wallis秩和检验对多组间细菌进行比较,筛选有统计学意义的变量。结果 3组细菌总检出率为73.0%,CRSwNP组、CRSsNP组和对照组细菌检出率分别为76.2%、68.6%、71.8%,3组比较差异无统计学意义(P=0.579);检出细菌以革兰阳性菌为主;检出率较高的细菌包括表皮葡萄球菌、假白喉棒状杆菌、金黄色葡萄球菌、流感嗜血杆菌、卡他莫拉菌;CRSwNP组与对照组流感嗜血杆菌检出率比较差异有统计学意义(13.5% vs 2.6%,P=0.009),但CRSsNP组和对照组该菌检出率比较差异无统计学意义(8.6% vs 2.6%,P=0.150);NonECRSwNP组和ECRSwNP组金黄色葡萄球菌检出率比较差异有统计学意义(9.6% vs 28.1%,P=0.017);NonECRSsNP组和ECRSsNP组金黄色葡萄球菌检出率差异无统计学意义(9.4% vs 16.7%,P=0.482)。结论 流感嗜血杆菌可能是CRSwNP的潜在病因;金黄色葡萄球菌可以促进CRSwNP嗜酸粒细胞炎症反应。Abstract: Objective To observe the microbiological characteristics and clinical correlation of chronic rhinosinusitis with different clinical phenotypes.Method One hundred and ninety-six patients with chronic rhinosinusitis(CRS) underwent nasal endoscopic surgery, including 126 patients with Chronic rhinosinusitis with nasal polyps(CRSwNP) and 70 patients with chronic rhinosinusitis without nasal polyps(CRSsNP); 78 patients with nasal septum deviation(control group) were enrolled. The nasal discharge samples were collected before operation, and the bacteria were isolated and identified by the traditional culture method. The bacteria were compared between the two groups by Pearson chi-square test or Fisher exact test, and the bacteria were compared between groups by Kruskal-Wallis rank sum test. Out statistically significant variables(P < 0.05).Result The total bacterial detection rate was 73.0% in the three groups, 76.2% in the CRSwNP group, 68.6% in the CRSsNP group and 71.8% in the control group, respectively(P=0.579). The detection rate of the bacteria was mainly Gram-positive bacteria. The higher detection rate included: Staphylococcus epidermidis, Pseudodiphtheria, Staphylococcus aureus, Haemophilus influenzaemola, Haemella influenzaemola. The detection rate of Haemophilus influenzae in the CRSwNP group and the control group(13.5% vs 2.6%, P=0.009), but there were statistical differences CRSsNP.There was no statistically significant difference in the detection rate of the bacteria(8.6% vs 2.6%, P=0.15) between the CRSsNP group and the control group; The difference of staphylococcus aureus detection rate between NonECRSwNP group and ECRSwNP group was statistically significant (9.6% vs 28.1%, P=0.017).There was no significant difference in staphylococcus aureus detection rate between NonECRSsNP group and ECRSsNP group (9.4% vs 16.7%, P=0.482).Conclusion Haemophilus influenzae may be a potential cause of CRSwNP; S. aureus may promote the eosinophilic granulocyte inflammatory response to CRSwNP.
-
Key words:
- sinusitis /
- microbiology /
- pathogenesis
-

-
表 1 CRSwNP组、CRSsNP组和对照组细菌培养的分离率
例(%) CRSwNP组
(n=126)CRSsNP组
(n=70)对照组
(n=78)P 阳性 96(76.2) 48(68.6) 56(71.8) 0.579 革兰阳性菌检出标本数 79(62.7) 39(55.7) 53(68.0) 0.307 革兰阴性菌检出标本数 32(25.4) 14(20.0) 11(14.1) 0.152 表 2 CRSwNP组、CRSsNP组和对照组标本中不同细菌种类的数量
例 组别 细菌菌属 Z P 0种 1种 2种 3种 4种 CRSwNP组 30 56 35 5 0 CRSsNP组 22 28 19 1 0 1.577 0.454 对照组 22 38 15 3 0 表 3 3组细菌检出率比较
例(%) 项目 CRSwNP组
(n=126)CRSsNP
(n=70)对照组
(n=78)P 革兰阳性菌 表皮葡萄球菌 37(29.4) 20(28.6) 29(37.2) 0.425 假白喉棒状杆菌 12(9.5) 6(8.6) 6(7.7) 0.902 金黄色葡萄球菌 18(14.3) 7(10.0) 10(12.8) 0.69 接近棒状杆菌 7(5.6) 1(1.4) 2(2.6) 0.382 肺炎链球菌 5(4.0) 2(2.9) 3(3.9) 1 草绿色链球菌 5(4.0) 3(4.3) 2(2.6) 0.845 懒惰狡诈颗粒菌 5(4.0) 3(4.3) 0 0.168 拥挤棒状杆菌 4(3.2) 4(5.7) 6(7.7) 0.312 纹带棒状杆菌 2(1.6) 0 0 0.501 沃氏葡萄球菌 2(1.6) 0 0 0.501 人皮肤杆菌 1(0.8) 0 0 1 藤黄微球菌 1(0.8) 0 0 1 克氏葡萄球菌 1(0.8) 0 1(1.3) 1 星座链球菌 1(0.8) 2(2.9) 1(1.3) 0.587 奥斯陆摩拉菌 1(0.8) 0 0 1 溶血葡萄球菌 1(0.8) 1(1.4) 2(2.6) 0.813 巴斯德葡萄球菌 1(0.8) 0 0 1 化脓性链球菌 1(0.8) 0 0 1 科氏葡萄球菌解脲亚种 0 1(1.4) 0 0.255 科氏葡萄球菌科氏亚种 0 1(1.4) 0 0.255 啮蚀艾肯菌 0 1(1.4) 0 0.255 头状葡萄球菌头状亚种 0 0 2(2.6) 0.145 人葡萄球菌 0 1(1.4) 2(2.6) 0.156 革兰阴性菌 流感嗜血杆菌 17(13.5)1) 6(8.6) 2(2.6) 0.031 卡他莫拉菌 12(9.5) 4(5.7) 4(5.1) 0.422 不液化莫拉菌 1(0.8) 1(1.4) 2(2.6) 0.813 铜绿假单胞菌 1(0.8) 0 0 1 非发酵棒杆菌 1(0.8) 0 0 1 克氏柠檬酸杆菌 1(0.8) 0 0 1 奈瑟菌 1(0.8) 1(1.4) 1(1.3) 1 多杀巴斯德菌 1(0.8) 0 0 1 产气肠杆菌 1(0.8) 0 1(1.3) 1 鲍曼不动杆菌 0 1(1.4) 0 1 琼氏不动杆菌 0 1(1.4) 1(1.3) 0.255 脲放线杆菌 0 1(1.4) 0 0.291 真菌 0 1(1.4) 0 0.255 与对照组比较,1)P < 0.05。 表 4 黏膜嗜酸粒细胞浸润对CRSwNP组和CRSsNP组细菌分布的影响
例(%) 细菌种类 CRSwNP组(n=126) P CRSsNP组(n=70) P NonECRSwNP
(n=94)ECRSwNP
(n=32)NonECRSsNP
(n=64)ECRSsNP
(n=6)凝固酶阴性葡萄球菌 表皮葡萄球菌 27(28.7) 10(31.3) 0.766 18(28.1) 2(33.3) 1.000 其他凝固酶阴性葡萄球菌 5(5.3) 0 0.328 3(4.7) 1(16.7) 0.304 流感嗜血杆菌 14(14.9) 3(9.4) 0.557 6(9.4) 0 1.000 卡他布兰汉菌 10(11.7) 2(6.3) 0.729 4(6.3) 0 1.000 金黄色葡萄球菌 9(9.6) 9(28.1) 0.017 6(9.4) 1(16.7) 0.482 革兰阳性棒状杆菌 20(21.3) 5(15.6) 0.489 10(15.6) 1(16.7) 1.000 肺炎链球菌 4(4.3) 1(3.1) 1.000 2(3.1) 0 1.000 草绿色链球菌 3(3.2) 2(6.3) 0.6 3(4.7) 0 1.000 铜绿假单胞菌 1(1.1) 0 1.000 0 0 - 化脓性链球菌 1(1.1) 0 1.000 0 0 - 鲍曼不动杆菌 0 0 - 1(1.6) 0 1.000 凝固酶阴性葡萄球菌包括:表皮葡萄球菌、科氏葡萄球菌解脲亚种、科氏葡萄球菌科氏亚种、人葡萄球菌、溶血葡萄球菌、沃氏葡萄球菌、克氏葡萄球菌、巴斯德葡萄球菌等;大部分凝固酶阴性葡萄球菌正常情况下无致病能力;革兰阳性棒状杆菌包括:假白喉棒状杆菌、接近棒状杆菌、拥挤棒状杆菌、纹带棒状杆菌。 表 5 内镜鼻窦手术病史对CRSwNP组、CRSsNP组细菌分布的影响
例(%) 细菌种类 CRSwNP组(n=126) P CRSsNP组(n=70) P 再次手术组
(n=23)初次手术组
(n=103)再次手术组
(n=10)初次手术组
(n=60)凝固酶阴性葡萄球菌 表皮葡萄球菌 7(30.4) 30(29.1) 0.901 4(40.0) 16(26.7) 0.456 其他凝固酶阴性葡萄球菌 0 5(4.9) 0.584 0 4(6.7) 1.000 流感嗜血杆菌 2(8.7) 15(14.6) 0.736 2(20.0) 4(6.7) 0.202 卡他布兰汉菌 4(17.4) 8(7.8) 0.230 1(10.0) 3(5.0) 0.468 金黄色葡萄球菌 5(21.7) 13(12.6) 0.321 1(10.0) 6(10.0) 1.000 革兰阳性棒状杆菌 3(13.0) 12(11.7) 1.000 1(10.0) 10(16.7) 1.000 肺炎链球菌 0 5(4.9) 0.584 1(10.0) 1(1.7) 0.267 草绿色链球菌 1(4.3) 4(3.9) 1.000 1(10.0) 2(3.3) 0.375 铜绿假单胞菌 0 1(1.0) 1.000 0 0 - 化脓性链球菌 1(4.3) 0 0.183 0 0 - 鲍曼不动杆菌 0 0 - 0 1(1.7) 1.000 表 6 AR对CRSsNP、CRSwNP、对照组细菌分布的影响
例(%) 细菌种类 CRSwNP组(n=126) P CRSsNP组(n=70) P 对照组(n=78) P 是
(n=28)否
(n=98)是
(n=16)否
(n=54)是
(n=16)否
(n=62)凝固酶阴性葡萄球菌 表皮葡萄球菌 11(39.3) 26(26.5) 0.191 7(43.8) 13(24.1) 0.206 8(50) 21(33.9) 0.234 其他凝固酶阴性葡萄球菌 2(7.1) 3(11.5) 0.308 0 4(7.4) 0.567 1(6.3) 6(9.7) 1.000 流感嗜血杆菌 6(21.4) 11(11.2) 0.208 2(12.5) 4(7.4) 0.614 1(6.3) 1(1.6) 0.37 卡他布兰汉菌 2(7.1) 10(10.2) 1.000 0 4(7.4) 0.567 1(6.3) 3(4.8) 1.000 金黄色葡萄球菌 9(32.1) 9(9.2) 0.005 2(12.5) 5(9.3) 0.655 2(12.5) 8(12.9) 1.000 革兰阳性棒状杆菌 4(14.3) 11(11.2) 0.741 2(12.5) 9(16.7) 1.000 4(25.0) 10(16.1) 0.469 肺炎链球菌 1(3.6) 4(4.1) 1.000 1(6.3) 1(1.9) 0.407 1(6.3) 2(3.2) 0.503 草绿色链球菌 1(3.6) 4(4.1) 1.000 1(6.3) 2(3.7) 0.547 0 2(3.2) 1.000 铜绿假单胞菌 1(3.6) 0 0.222 0 0 - 0 0 - 化脓性链球菌 0 1(1.0) 1.000 0 0 - 0 0 - 鲍曼不动杆菌 0 0 - 0 1(1.9) 1.000 0 0 - 表 7 吸烟对CRSwNP、CRSsNP和对照组细菌分布的影响
例(%) 细菌种类 CRSwNP(n=126) P CRSsNP组(n=70) P 对照组(n=78) P 是
(n=40)否
(n=86)是
(n=17)否
(n=53)是
(n=6)否
(n=72)凝固酶阴性葡萄球菌 表皮葡萄球菌 13(32.5) 24(27.9) 0.598 5(29.4) 15(28.3) 1.000 0 29(40.3) 0.079 其他凝固酶阴性葡萄球菌 2(5.0) 3(3.5) 0.652 0 4(7.5) 0.566 2(33.3) 5(6.9) 0.088 流感嗜血杆菌 4(10.0) 13(15.1) 0.434 0 6(11.3) 0.324 0 2(2.8) 1.000 卡他布兰汉菌 5(12.5) 7(8.1) 0.518 2(11.8) 2(3.8) 0.246 0 4(5.6) 1.000 金黄色葡萄球菌 5(12.5) 13(15.1) 0.696 2(11.8) 5(9.4) 1.000 0 10(13.9) 1.000 革兰阳性棒状杆菌 9(22.5) 16(18.6) 0.61 2(11.8) 9(17.0) 1.000 2(33.3) 12(16.7) 0.293 肺炎链球菌 0 5(5.8) 0.177 1(5.9) 1(1.9) 0.429 0 3(4.2) 1.000 草绿色链球菌 2(5.0) 3(3.5) 0.625 0 3(5.7) 1.000 0 2(2.8) 1.000 铜绿假单胞菌 1(2.5) 0 0.317 0 0 - 0 0 - 化脓性链球菌 0 1(1.1) 1.000 0 0 - 0 0 - 鲍曼不动杆菌 0 0 - 1(5.9) 0 0.243 0 0 - 吸烟者:最近1年内吸烟量≥20支/d;非吸烟者:取样前吸烟总量 < 50支,但不排外被动吸烟情况,吸烟后又戒烟者不纳入本研究。 -
[1] Shi JB, Fu QL, Zhang H, et al. Epidemiology of chronic rhinosinusitis: results from a cross-sectional survey in seven Chinese cities[J]. Allergy, 2015, 70(5): 533-539. doi: 10.1111/all.12577
[2] Sousa CA, César CL, Barros MB, et al. Prevalence of chronic obstructive pulmonary disease and risk factors in São Paulo, Brazil, 2008-2009[J]. Rev Saude Publica, 2011, 45(5): 887-896. doi: 10.1590/S0034-89102011005000051
[3] Hoggard M, Wagner Mackenzie B, Jain R, et al. Chronic Rhinosinusitis and the Evolving Understanding of Microbial Ecology in Chronic Inflammatory Mucosal Disease[J]. Clin Microbiol Rev, 2017, 30(1): 321-348. doi: 10.1128/CMR.00060-16
[4] Smeekens SP, Huttenhower C, Riza A, et al. Skin microbiome imbalance in patients with STAT1/STAT3 defects impairs innate host defense responses[J]. J Innate Immun, 2014, 6(3): 253-262. doi: 10.1159/000351912
[5] Khalid AN, Hunt J, Perloff JR, et al. The role of bone in chronic rhinosinusitis[J]. Laryngoscope, 2002, 112(11): 1951-1957. doi: 10.1097/00005537-200211000-00008
[6] Akdis CA, Bachert C, Cingi C, et al. Endotypes and phenotypes of chronic rhinosinusitis: a PRACTALL document of the European Academy of Allergy and Clinical Immunology and the American Academy of Allergy, Asthma & Immunology[J]. J Allergy Clin Immunol, 2013, 131(6): 1479-1490. doi: 10.1016/j.jaci.2013.02.036
[7] Kennedy JL, Borish L. Chronic rhinosinusitis and antibiotics: the good, the bad, and the ugly[J]. Am J Rhinol Allergy, 2013, 27(6): 467-472. doi: 10.2500/ajra.2013.27.3960
[8] Hauser LJ, Feazel LM, Ir D, et al. Sinus culture poorly predicts resident microbiota[J]. Int Forum Allergy Rhinol, 2015, 5(1): 3-9. doi: 10.1002/alr.21428
[9] Worrall G. Acute sinusitis[J]. Can Fam Physician, 2011, 57(5): 565-567.
[10] Seiberling KA, Conley DB, Tripathi A, et al. Superantigens and chronic rhinosinusitis: detection of staphylococcal exotoxins in nasal polyps[J]. Laryngoscope, 2005, 115(9): 1580-1585. doi: 10.1097/01.mlg.0000168111.11802.9c
[11] Yu RL, Dong Z. Proinflammatory impact of Staphylococcus aureus enterotoxin B on human nasal epithelial cells and inhibition by dexamethasone[J]. Am J Rhinol Allergy, 2009, 23(1): 15-20. doi: 10.2500/ajra.2009.23.3252
[12] Bachert C, Gevaert P, Holtappels G, et al. Total and specific IgE in nasal polyps is related to local eosinophilic inflammation[J]. J Allergy Clin Immunol, 2001, 107(4): 607-614. doi: 10.1067/mai.2001.112374
[13] 孟昕君. 慢性鼻窦炎与细菌感染[J]. 临床耳鼻咽喉头颈外科杂志, 2010, 24(8): 382-384. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201008023.htm
[14] 魏洪政, 王向东, 朱敏, 等. 不同外周血嗜酸粒细胞表型的慢性鼻-鼻窦炎伴鼻息肉的微生物学研究[J]. 临床耳鼻咽喉头颈外科杂志, 2017, 31(5): 338-342. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201705003.htm
[15] Liu Q, Lu X, Bo M, et al. The microbiology of chronic rhinosinusitis with and without nasal polyps[J]. Acta Otolaryngol, 2014, 134(12): 1251-1258. doi: 10.3109/00016489.2013.879737
[16] Rasmussen TT, Kirkeby LP, Poulsen K, et al. Resident aerobic microbiota of the adult human nasal cavity[J]. APMIS, 2000, 108(10): 663-675. doi: 10.1034/j.1600-0463.2000.d01-13.x
[17] Chalermwatanachai T, Vilchez-Vargas R, Holtappels G, et al. Chronic rhinosinusitis with nasal polyps is characterized by dysbacteriosis of the nasal microbiota[J]. Sci Rep, 2018, 8(1): 7926. doi: 10.1038/s41598-018-26327-2
[18] Hoggard M, Biswas K, Zoing M, et al. Evidence of microbiota dysbiosis in chronic rhinosinusitis[J]. Int Forum Allergy Rhinol, 2017, 7(3): 230-239. doi: 10.1002/alr.21871
[19] Poole J, Foster E, Chaloner K, et al. Analysis of nontypeable haemophilus influenzae phase-variable genes during experimental human nasopharyngeal colonization[J]. J Infect Dis, 2013, 208(5): 720-727. doi: 10.1093/infdis/jit240
[20] Cui X, Chen H, Rui Y, et al. Two-stage open reduction and internal fixation versus limited internal fixation combined with external fixation: a meta-analysis of postoperative complications in patients with severe Pilon fractures[J]. J Int Med Res, 2018, 46(7): 2525-2536. doi: 10.1177/0300060518776099
[21] Frank DN, Feazel LM, Bessesen MT, et al. The human nasal microbiota and Staphylococcus aureus carriage[J]. PLoS One, 2010, 5(5): e10598. doi: 10.1371/journal.pone.0010598
[22] Valera F, Ruffin M, Adam D, et al. Staphylococcus aureus impairs sinonasal epithelial repair: Effects in patients with chronic rhinosinusitis with nasal polyps and control subjects[J]. J Allergy Clin Immunol, 2019, 143(2): 591-603.e3. doi: 10.1016/j.jaci.2018.05.035
[23] Calus L, Derycke L, Dullaers M, et al. IL-21 Is Increased in Nasal Polyposis and after Stimulation with Staphylococcus aureus Enterotoxin B[J]. Int Arch Allergy Immunol, 2017, 174(3-4): 161-169. doi: 10.1159/000481435
[24] Lan F, Zhang N, Holtappels G, et al. Staphylococcus aureus Induces a Mucosal Type 2 Immune Response via Epithelial Cell-derived Cytokines[J]. Am J Respir Crit Care Med, 2018, 198(4): 452-463. doi: 10.1164/rccm.201710-2112OC
[25] Dlugaszewska J, Leszczynska M, Lenkowski M, et al. The pathophysiological role of bacterial biofilms in chronic sinusitis[J]. Eur Arch Otorhinolaryngol, 2016, 273(8): 1989-1994. doi: 10.1007/s00405-015-3650-5
-

| 引用本文: | 刘肖, 刘红兵, 李春花, 等. 不同临床表型的慢性鼻窦炎的微生物学研究[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(9): 805-810. doi: 10.13201/j.issn.2096-7993.2020.09.009 |
| Citation: | LIU Xiao, LIU Hongbing, LI Chunhua, et al. Microbiology of chronic rhinosinusitis with different clinical phenotypes[J]. J Clin Otorhinolaryngol Head Neck Surg, 2020, 34(9): 805-810. doi: 10.13201/j.issn.2096-7993.2020.09.009 |
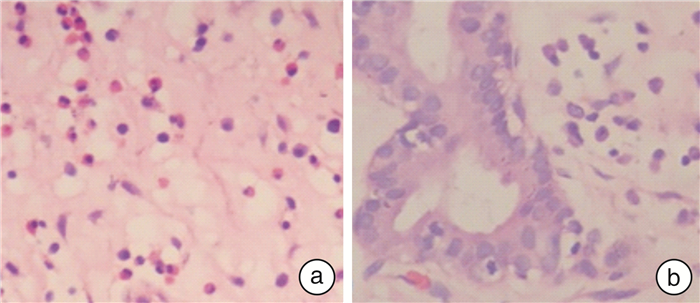
- Figure 1.



 下载:
下载: