-
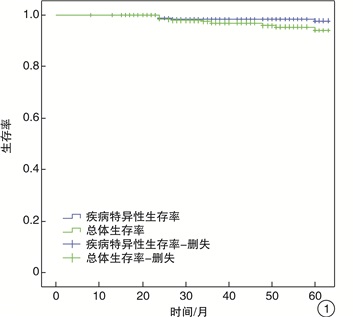
摘要: 目的 分析黏膜波变化与早期喉癌浸润层次的关系从而指导术者选择相应的术式。方法 回顾性分析因原发声门型喉鳞状细胞癌接受单纯CO2激光治疗早期T1a期无前连合侵犯患者的临床资料。结果 本研究共筛选出320例患者,其中有22例术前嗓音评估提示黏膜波轻度减低,49例黏膜波中度减低,151例黏膜波重度减低,98例黏膜波提示消失。术后病理显示肿瘤局限于上皮层的患者16例,其中15例接受Ⅲ型激光手术治疗,1例接受Ⅳ型激光手术;术后病理显示肿瘤浸润至固有层的患者189例,其中148例接受Ⅲ型激光手术,41例接受Ⅳ型激光手术;病理显示肿瘤浸润至声带肌层的患者115例,77例接受Ⅲ型激光手术,38例接受Ⅳ型激光手术。按Kaplan-Meier法分析显示入选患者5年总体生存率为94.0%,5年疾病特异性生存率为98.4%,5年局部区域控制率为91.2%。黏膜波变化与肿瘤浸润层次有显著相关性;肿瘤浸润至固有层的患者接受Ⅲ、Ⅳ型激光术式治疗,其5年总体生存率及5年局部区域控制率无明显差异;肿瘤浸润至肌层的患者接受Ⅲ、Ⅳ型激光术式治疗5年总体生存率及5年局部区域控制率无明显差异。结论 本研究显示黏膜波的变化可在一定程度上提示肿瘤浸润程度并指导术中术式,怀疑为喉癌的患者术前黏膜波提示中度-重度减低或消失时,为保证基底切缘干净至少应切至肌层,黏膜波消失的喉癌患者提示肿瘤可能浸润至肌层,Ⅲ、Ⅳ型激光术式对其预后无明显影响。Abstract: Objective Analyze the relationship between the change of mucosal wave and the infiltrating level of early laryngeal carcinoma so as to guide the cordectomy.Method Retrospective research on patients of 1a stage without anterior commissure invasion who received simple CO2 laser therapy because of primary glottic laryngeal squamous cell carcinoma.Result Records of 320 patients including 22 patients who have slightly reduced according to the mucosal wave prompts before operation, 49 patients mucosal wave moderately reduced, 151 patients mucosal wave severely reduced, and 98 patients have mucosal wave disappeared according to stroboscopic assessment. Post-pathological evidence shows that 16 patients had their tumor infiltration into the epithelial layer, of which, 15 received the Ⅲ type laser surgery, 1 patient received the Ⅳ type laser surgery; 189 patients had their tumor infiltration into the lamina propria, of which, 148 received the Ⅲ type laser surgery, 41 received the Ⅳ type laser surgery; and 115 patients had their tumor infiltration into the vocal cord muscle layer, of which, 77 received the Ⅲ type laser surgery, 38 received the Ⅳ type laser surgery. Analyzed according to the Kaplan-Meier method, it shows that their five-year overall survival rate was 94.0%, the five-year disease-specific survival rate was 98.4%; and five-year local-region control rate was 91.2%. Change of the mucosal wave and the tumor infiltrating level have significant correlation; patients whose tumor infiltration had reached the lamina propria received the Ⅲ and Ⅳ type laser surgical treatment, their five-year overall survival rate and their five-year local-region area control rate have no obvious difference; patients whose tumor infiltration have reached the muscular layer received the Ⅲ and Ⅳ type laser surgical treatment, their five-year overall survival rate and their five-year local-region area control rate have no significant difference.Conclusion This research shows that, change of the mucosal wave can, to a certain extent, prompt the tumor infiltration degree and guide in operation; for patients who are suspected of laryngeal carcinoma, when mucosal wave before operation prompts moderate-sever reduction or disappearance, to ensure bottom incisal margin clean, it should be cut at least to the muscular layer; for laryngeal cancer patients whose infiltrating mucosal wave disappears, it prompts that the tumor may have infiltrated to the muscular layer, and the Ⅲ and Ⅳ type laser surgery will have no significant prognostic influence.
-

-
[1] Mendelsohn AH, Remacle M, Courey MS, et al. The diagnostic role of high-speed vocal fold vibratory imaging[J]. J Voice, 2013, 27(5): 627-631. doi: 10.1016/j.jvoice.2013.04.011
[2] Krausert CR, Olszewski AE, Taylor LN, et al. Mucosal wave measurement and visualization techniques[J]. J Voice, 2011, 25(4): 395-405. doi: 10.1016/j.jvoice.2010.02.001
[3] Inwald EC, Döllinger M, Schuster M, et al. Multiparametric analysis of vocal fold vibrations in healthy and disordered voices in high-speed imaging[J]. J Voice, 2011, 25(5): 576-590. doi: 10.1016/j.jvoice.2010.04.004
[4] Woo P. Quantification of videostrobolaryngoscopic findings——measurements of the normal glottal cycle[J]. Laryngoscope, 2010, 106(S79): 1-27.
[5] 黄志刚, 韩德民, 倪鑫, 等. 声带癌T1病变的CO2激光治疗[J]. 耳鼻咽喉头颈外科, 1996, 3(3): 152-154. https://www.cnki.com.cn/Article/CJFDTOTAL-EBYT603.012.htm
[6] Breda E, Catarino R, Monteiro E. Transoral laser microsurgery for laryngeal carcinoma: Survival analysis in a hospital-based population[J]. Head Neck, 2015, 37(8): 1181-1186. doi: 10.1002/hed.23728
[7] Spielmann PM, Majumdar S, Morton RP. Quality of life and functional outcomes in the management of early glottic carcinoma: a systematic review of studies comparing radiotherapy and transoral laser microsurgery[J]. Clin Otolaryngol, 2010, 35(5): 373-382. doi: 10.1111/j.1749-4486.2010.02191.x
[8] Mendenhall WM, Werning JW, Hinerman RW, et al. Management of T1-T2glottic carcinomas[J]. Cancer, 2010, 100(9): 1786-1792.
[9] Canis M, Ihler F, Martin A, et al. Transoral laser microsurgery for T1a glottic cancer: Review of 404 cases[J]. Head Neck, 2015, 37(6): 889-895. doi: 10.1002/hed.23688
[10] Remacle M, Eckel HE, Antonelli A, et al. Endoscopic cordectomy. A proposal for a classification by the Working Committee, European Laryngological Society[J]. Eur Arch Otorhinolaryngol, 2000, 257(4): 227-231. doi: 10.1007/s004050050228
[11] Rucci L, Romagnoli P, Scala J. CO2 laser therapy in Tis and T1 glottic cancer: indications and results[J]. Head Neck, 2010, 32(3): 392-398.
[12] Mortuaire G, Francois J, Wiel E, et al. Local Recurrence after CO2 Laser Cordectomy for Early Glottic Carcinoma[J]. Laryngoscope, 2010, 116(1): 101-105.
[13] Colden D, Zeitels SM, Hillman RE, et al. Stroboscopic assessment of vocal fold keratosis and glottic cancer[J]. Ann Otol Rhinol Laryngol, 2001, 110(4): 293-298. doi: 10.1177/000348940111000401
[14] Piazza C, Mangili S, Bon FD, et al. Quantitative analysis of videokymography in normal and pathological vocal folds: a preliminary study[J]. Eur Arch Otorhinolaryngol, 2012, 269(1): 207-212. doi: 10.1007/s00405-011-1780-y
[15] Bajaj Y, Uppal S, Sharma RK, et al. Evaluation of voice and quality of life after transoral endoscopic laser resection of early glottic carcinoma[J]. J Laryngol Otol, 2011, 125(7): 706-713. doi: 10.1017/S002221511100065X
-

| 引用本文: | 丁硕, 黄俊伟, 郭伟, 等. 黏膜波变化对早期喉癌激光治疗的指导[J]. 临床耳鼻咽喉头颈外科杂志, 2020, 34(9): 769-772. doi: 10.13201/j.issn.2096-7993.2020.09.001 |
| Citation: | DING Shuo, HUANG Junwei, GUO Wei, et al. Guidance of laser therapy for early laryngeal carcinoma by mucosal wave changes[J]. J Clin Otorhinolaryngol Head Neck Surg, 2020, 34(9): 769-772. doi: 10.13201/j.issn.2096-7993.2020.09.001 |
- Figure 1.
- Figure 2.
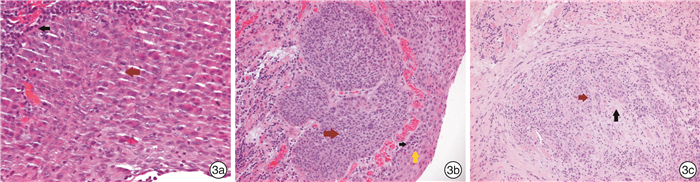
- Figure 3.



 下载:
下载: