A study on the quality of life and mental health of sinusitis patients with olfactory disorders
-
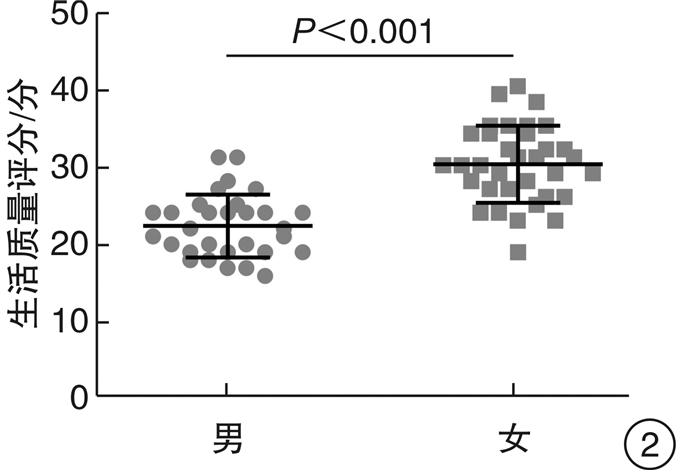
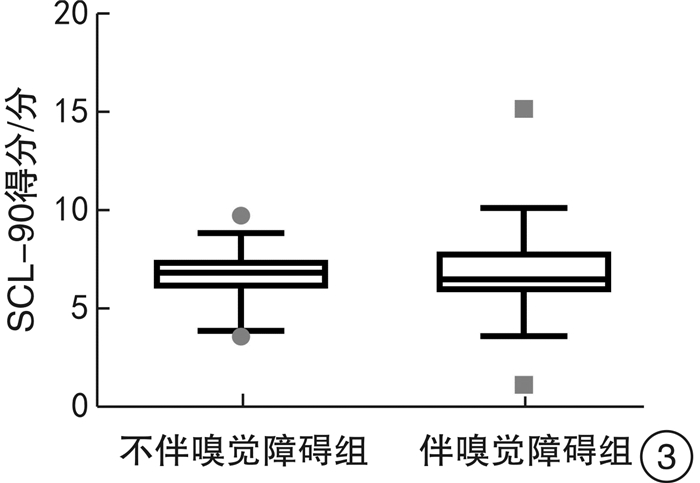
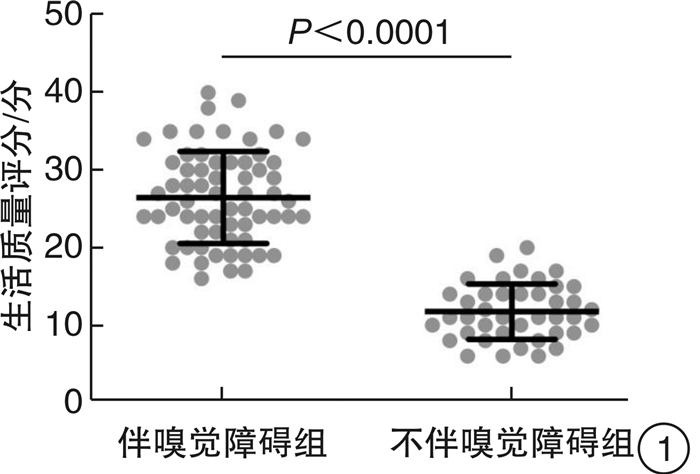
摘要: 目的 研究伴与不伴鼻息肉CRS患者嗅觉障碍发生率及伴有嗅觉障碍的CRS患者对生活质量及心理健康的影响。方法 将随机选取的105例CRS患者根据Sniffin's Sticks嗅觉检查结果分为伴嗅觉障碍组和不伴嗅觉障碍组,分别行嗅觉障碍生存质量量表-生存质量部分、SCL-90症状自评量表评分。结果 在CRS患者中,伴鼻息肉较不伴鼻息肉嗅觉障碍的发生率显著增高(χ2=37.133,P<0.001);嗅觉障碍生存质量量表-生存质量部分评分,伴嗅觉障碍组生存质量评分(26.5±5.9)显著高于不伴嗅觉障碍组(11.76±3.58)(t=14.30,P<0.0001);伴嗅觉障碍女性患者生活质量评分(30.2±4.9)显著高于男性(22.3±4.0)(P<0.001);伴嗅觉障碍的CRS患者(64例)SCL-90评分为6.6(6.0~8.0),不伴嗅觉障碍的CRS患者(41例)SCL-90评分为7.0(6.2~7.6),2组间比较差异无统计学意义(P>0.05)。结论 CRS伴鼻息肉患者发生嗅觉障碍的风险显著高于不伴鼻息肉者;伴嗅觉障碍的CRS患者生活质量较不伴嗅觉障碍的CRS患者明显下降,且女性较男性对生活质量的影响更明显;伴嗅觉障碍的CRS患者对心理健康无显著影响。Abstract: Objective The aim of this study is to investigate the incidence of dysosmia in patients with and without nasal polyps, and the impact of dysosmia on the quality of life and mental health in patients with Sinusitis.Method A total of 105 randomly selected patients with Sinusitis were divided into two groups based on the results of the Sniffin's Sticks olfactory examination: The dysosmia group and the non dysosmia group, the quality of life (Qol) of olfaction quality of life scale and SCL-90 symptom checklist-90(SCL-90) were scored respectively.Result The incidence of olfactory disorders in chronic sinusitis patients with nasal polyps was significantly higher than those without nasal polyps(χ2=37.133, P < 0.001). The quality of life score of the olfactory disturbance scale the quality of life score of the olfactory disturbance group(26.5±5.9) was significantly higher than that of the non olfactory disturbance group(11.76±3.58)(t=14.30, P < 0.0001). Life quality score(30.2±4.9) of female patients with olfactory dysfunction was significantly higher than that of male patients(22.3±4.0)(P < 0.001), The score of SCL-90 of chronic sinusitis patients with olfactory dysfunction(n=64) is 6.6(6.0-8.0), while the score of SCL-90 of chronic sinusitis patients without olfactory dysfunction(n=41) is 7.0(6.2-7.6), and there was no significant difference between the two groups(P>0.05).Conclusion The risk of dysosmia in patients with Sinusitis polyps was significantly higher than that in patients without nasal polyps, and the quality of life in patients with Sinusitis was significantly lower than that in patients without sinusitis, women also had a greater impact on their quality of life than men, and Sinusitis patients with dysosmia had no significant impact on their mental health.
-
Key words:
- chronic rhinosinusitis /
- olfactory disorders /
- quality of life /
- mental health
-

-
[1] Ruggiero GF, Wick JY. Olfaction: New Understandings, Diagnostic Applications[J]. Consult Pharm, 2016, 31(11): 624-632. doi: 10.4140/TCP.n.2016.624
[2] Liu G, Zong G, Doty RL, et al. Prevalence and risk factors of taste and smell impairment in a nationwide representative sample of the US population: a cross-sectional study[J]. BMJ Open, 2016, 6(11): e013246. doi: 10.1136/bmjopen-2016-013246
[3] Vennemann MM, Hummel T, Berger K. The association between smoking and smell and taste impairment in the general population[J]. J Neurol, 2008, 255(8): 1121-1126. doi: 10.1007/s00415-008-0807-9
[4] Brämerson A, Johansson L, Ek L, et al. Prevalence of olfactory dysfunction: the skövde population-based study[J]. Laryngoscope, 2004, 114(4): 733-737. doi: 10.1097/00005537-200404000-00026
[5] Huang Z, Huang S, Cong H, et al. Smell and Taste Dysfunction Is Associated with Higher Serum Total Cholesterol Concentrations in Chinese Adults[J]. J Nutr, 2017, 147(8): 1546-1551. doi: 10.3945/jn.117.250480
[6] Rawal S, Hoffman HJ, Bainbridge KE, et al. Prevalence and Risk Factors of Self-Reported Smell and Taste Alterations: Results from the 2011-2012 US National Health and Nutrition Examination Survey(NHANES)[J]. Chem Senses, 2016, 41(1): 69-76. doi: 10.1093/chemse/bjv057
[7] Litvack JR, Fong K, Mace J, et al. Predictors of olfactory dysfunction in patients with chronic rhinosinusitis[J]. Laryngoscope, 2008, 118(12): 2225-2230. doi: 10.1097/MLG.0b013e318184e216
[8] Alobid I, Cardelus S, Benítez P, et al. Persistent asthma has an accumulative impact on the loss of smell in patients with nasalpolyposis[J]. Rhinology. 2011 Dec; 49(5): 519-524.
[9] Nordin S, Blomqvist EH, Olsson P, et al. Effects of smell loss on daily life and adopted coping strategies in patients with nasal polyposis with asthma[J]. Acta Otolaryngol, 2011, 131(8): 826-832. doi: 10.3109/00016489.2010.539625
[10] Yee KK, Pribitkin EA, Cowart BJ, et al. Neuropathology of the olfactory mucosa in chronic rhinosinusitis[J]. Am J Rhinol Allergy, 2010, 24(2): 110-120. doi: 10.2500/ajra.2010.24.3435
[11] Kern RC. Chronic sinusitis and anosmia: pathologic changes in the olfactory mucosa[J]. Laryngoscope, 2000, 110(7): 1071-1077. doi: 10.1097/00005537-200007000-00001
[12] Rombaux P, Mouraux A, Bertrand B, et al. Olfactory function and olfactory bulb volume in patients with postinfectious olfactory loss[J]. Laryngoscope, 2006, 116(3): 436-439. doi: 10.1097/01.MLG.0000195291.36641.1E
[13] 于焕新, 杭伟, 张金玲, 等. 阿尔茨海默病患者嗅觉功能以及嗅球体积和嗅沟深度的研究[J]. 临床耳鼻咽喉头颈外科杂志, 2015, 29(5): 444-447. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201505017.htm
[14] Malkarnekar NA, Behere RV, Bhandary RP, et al. Olfactory perceptual abnormality associated with vitamin B12 deficiency[J]. Psychosomatics, 2014, 55(3): 310-311. doi: 10.1016/j.psym.2013.06.007
[15] Han P, Winkler N, Hummel C, et al. Impaired brain response to odors in patients with varied severity of olfactory loss after traumatic brain injury[J]. J Neurol, 2018, 265(10): 2322-2332. doi: 10.1007/s00415-018-9003-8
[16] Atalar AÇ, Erdal Y, Tekin B, et al. Olfactory dysfunction in multiple sclerosis[J]. Mult Scler Relat Disord, 2018, 21: 92-96. doi: 10.1016/j.msard.2018.02.032
[17] Viguera C, Wang J, Mosmiller E, et al. Olfactory dysfunction in amyotrophic lateral sclerosis[J]. Ann Clin Transl Neurol, 2018, 19, 5(8): 976-981.
[18] Kohler CG, Moberg PJ, Gur RE, et al. Olfactory dysfunction in schizophrenia and temporal lobe epilepsy[J]. Neuropsychiatry Neuropsychol Behav Neurol, 2001, 14(2): 83-88.
[19] Rombaux P, Huart C, Levie P, et al. Olfaction in Chronic Rhinosinusitis[J]. Curr Allergy Asthma Rep, 2016, 16(5): 41-41. doi: 10.1007/s11882-016-0617-6
[20] Hur K, Choi JS, Zheng M, et al. Association of alterations in smell and taste with depression in older adults[J]. Laryngoscope Investig Otolaryngol, 2018, 3(2): 94-99. doi: 10.1002/lio2.142
-




 下载:
下载: