Analysis of the effect of endoscopic surgery combined with conventional surgery in Neuroblastoma
-
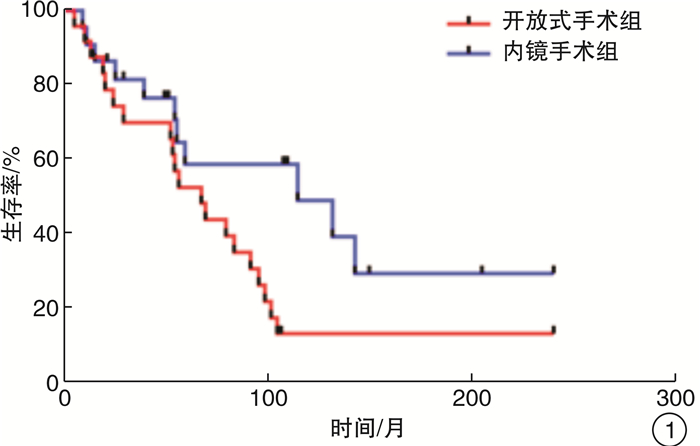
摘要: 目的 探讨内镜手术与传统手术联合放射治疗嗅神经母细胞瘤的疗效。方法 回顾分析43例接受手术联合放疗的嗅神经母细胞瘤患者疗效,按照手术方式分为内镜手术与传统手术,所有患者术后均接受放疗,放疗剂量60~70 Gy,对2组患者的5年生存率、局部复发时间进行比较,对比内镜手术与传统手术的治疗效果。结果 通过生存分析,开放手术组与内镜手术组5年总体生存率分别为50%和58%(P=0.560);局部复发率分别为44%与48%(P=0.288),平均复发时间分别为5.6个月与12.5个月(P=0.032)。结论 内镜手术与传统手术联合放疗治疗嗅神经母细胞瘤疗效无差异,且局部复发时间显著延长,在早期嗅神经母细胞瘤患者诊治中,鼻内镜手术治疗效果和患者生存治疗方面可能优于开放手术。Abstract: Objective The aim of this study is to evaluate the efficacy of endoscopic surgery and conventional surgery combined with radiotherapy in the treatment of Neuroblastoma.Method Forty-three patients with olfactory neuroblastoma undergoing surgery combined with radiotherapy were retrospectively analyzed. The patients were divided into endoscopic surgery and conventional surgery. All patients received postoperative radiotherapy at a dose of 60-70 Gy, the 5-year survival rate and local recurrence time of the two groups were compared, and the therapeutic effects of endoscopic surgery and traditional surgery were compared.Result Through survival analysis, the 5-year overall survival rates of the traditional surgery group and the endoscopic surgery group were 50% and 58% (P=0.560), the local recurrence rates were 44% and 48% (P=0.288), and the mean recurrence time was 5.6 months and 12.5 months (P=0.032).Conclusion There was no difference between endoscopic surgery and conventional surgery combined with radiotherapy in the treatment of Neuroblastoma, and the time of local recurrence was significantly prolonged. In early Neuroblastoma, endoscopic sinus surgery may be superior to open surgery in terms of efficacy and patient survival.
-
Key words:
- esthesioneuroblastoma /
- radiation therapy /
- treatment effect
-

-
[1] Palejwala SK, Sharma S, Le CH, et al. Complications of Advanced Kadish Stage Esthesioneuroblastoma: SingleInstitution Experienceand Literature Review[J]. Cureus, 2017, 9: e1245.
[2] Konuthula N, Iloreta A M, Miles B, et al. Prognostic significance of Kadish staging in esthesioneuroblastoma: An analysis of the NationalCancer Database[J]. Head Neck, 2017, 39: 1962-1968. doi: 10.1002/hed.24770
[3] 罗宁, 郭汝元. 嗅神经母细胞瘤23例临床分析[J]. 中国药物与临床, 2018, 18(3): 417-419. https://www.cnki.com.cn/Article/CJFDTOTAL-YWLC201803042.htm
[4] Folbe A, Herzallah I, Duvvuri U, et al. Endoscopic endonasal resection of esthesioneuroblastoma: a multicenter study[J]. Am J Rhinol Allergy, 2009, 23: 91-94. doi: 10.2500/ajra.2009.23.3269
[5] 孙敬武, 汪银凤, 郭涛, 等. 经鼻内镜切除侵犯前颅底鼻腔恶性肿瘤的疗效分析[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32(10): 778-781. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201810015.htm
[6] KöNig M S, Osnes T, Meling T R. Treatment of esthesioneuroblastomas[J]. Neurochirurgie, 2014, 60: 151-157. doi: 10.1016/j.neuchi.2014.03.007
[7] 文开学, 高颖, 赵菲. 妊娠28+周并发嗅神经母细胞瘤1例[J]. 临床耳鼻咽喉头颈外科杂志, 2017, 31(8): 75-76. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201708019.htm
[8] Khosla M, Pecci C, Do A, et al. Esthesioneuroblastoma with widespread distant metastasis: Case report and literature review[J]. Ear Nose Throat J, 2018, 97: E18-E21. doi: 10.1177/014556131809700905
[9] Klironomos G, Gonen L, Au K, et al. Endoscopic management of Esthesioneuroblastoma: Our experience and review of the literature[J]. J Clin Neurosci, 2018, 58: 117-123. doi: 10.1016/j.jocn.2018.09.011
[10] 黎高新, 周建波, 肖旭平, 等. 传统手术与鼻内镜辅助手术治疗嗅神经母细胞瘤19例分析[J]. 临床耳鼻咽喉头颈外科杂志, 2008, 22(11): 498-499. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH200811012.htm
[11] Castelnuovo P, Bignami M, Delù G, et al. Endonasal endoscopic resection and radiotherapy in olfactory neuroblastoma: our experience[J]. Head Neck, 2007, 29: 845-850. doi: 10.1002/hed.20610
[12] Zahedi FD, Gendeh BS, Husain S, et al. Ectopic Esthesioneuroblastoma of the Sphenoclivus: A Rare Entity[J]. Indian J Otolaryngol Head Neck Surg, 2017, 69: 125-129. doi: 10.1007/s12070-016-0978-0
[13] Marinelli JP, Janus JR, Van Gompel JJ, et al. Esthesioneuroblastoma with distant metastases: Systematic review & meta-analysis[J]. Head Neck, 2018, 40: 2295-2303. doi: 10.1002/hed.25209
[14] 朱歆洁, 陈智斌. 显微外科技术辅助鼻-颅底肿瘤切除的临床体会[J]. 临床耳鼻咽喉头颈外科杂志, 2018, 32(6): 452-456. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201806013.htm
[15] Zafereo ME, Fakhri S, Prayson R, et al. Esthesioneuroblastoma: 25-year experience at a single institution[J]. Otolaryngol Head Neck Surg, 2008, 138: 452-458. doi: 10.1016/j.otohns.2007.12.038
[16] 叶宇东, 邱前辉, 张水兴, 等. 原发鼻腔鼻窦恶性肿瘤内镜术后的长期疗效观察[J]. 临床耳鼻咽喉头颈外科杂志, 2015, 29(12): 1105-1110. https://www.cnki.com.cn/Article/CJFDTOTAL-LCEH201512016.htm
[17] Petruzzelli GJ, Howell JB, Pederson A, et al. Multidisciplinary treatment of olfactory neuroblastoma: Patterns of failure and management of recurrence[J]. Am J Otolaryngol, 2015, 36: 547-553. doi: 10.1016/j.amjoto.2015.02.008
[18] Devaiah AK, Andreoli MT. Treatment of esthesioneuroblastoma: a 16-year meta-analysis of 361 patients[J]. Laryngoscope, 2009, 119: 1412-1416. doi: 10.1002/lary.20280
[19] Yu Y, El-Sayed I H, Mcdermott MW, et al. Dural recurrence among esthesioneuroblastoma patients presenting with intracranial extension[J]. Laryngoscope, 2018, 128: 2226-2233. doi: 10.1002/lary.27126
-




 下载:
下载:
